ARLINGTON, Va. — The pharmacy industry and National Association of Chain Drug Stores are at an inflection point, says NACDS president and chief executive officer Steve Anderson.
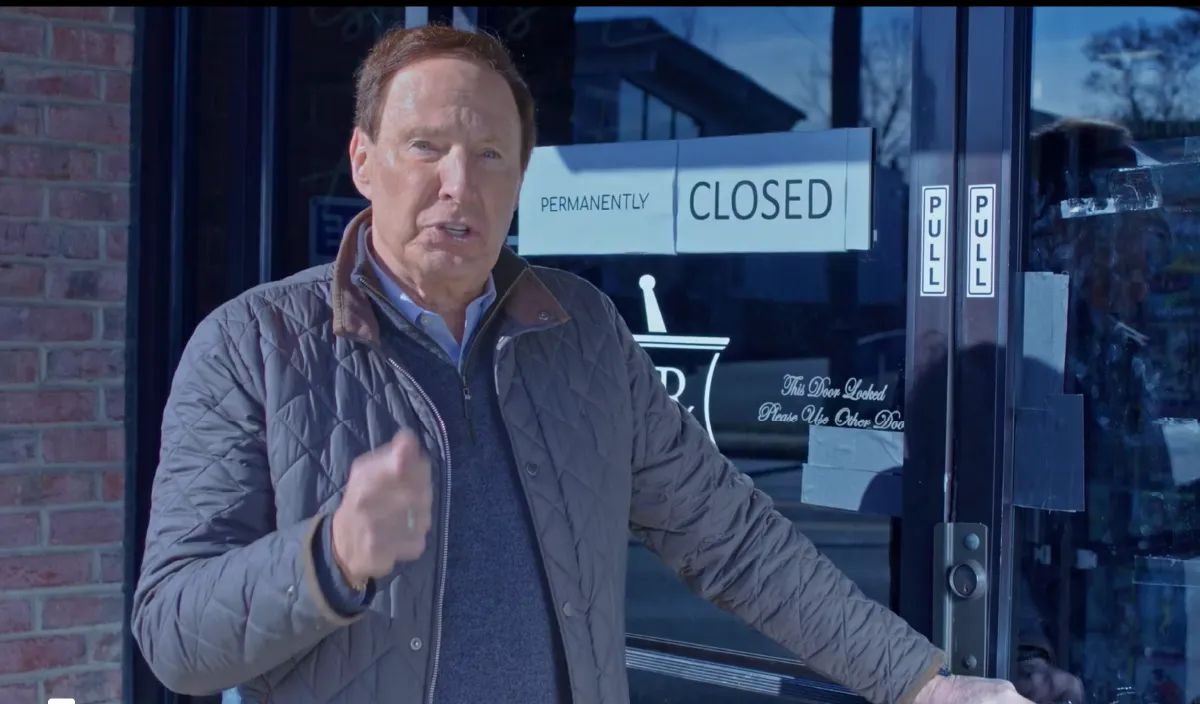
Anderson warned in a TV ad that PBMs were making it impossible for pharmacies to stay open.
With momentum building for pharmacy benefit manager reform and the growing recognition that pharmacists are integral to value-based retail health care, the industry and association are poised for a dramatic new era, he says.
The imminence of momentous change is hardly coincidental, Anderson adds, saying that NACDS’ board was looking ahead to such developments as far back as the height of the pandemic. Even as the focus was on COVID testing and vaccinating at pharmacies, “we were already having discussions at the board level about what was coming. What was the next big thing that we needed to be working on?”
Given such foresight, “the future of retail health care and NACDS is very bright,” he says. “It’s going to be an exciting time.”
Anderson is optimistic despite the dysfunction of Congress, which has stalled passage of PBM reform and provider status legislation for pharmacists. Several such bills have emerged in the House and Senate, including PBM reform legislation approved by the Senate Finance Committee by a vote of 26-0. They are falling short of enactment because they are getting bogged down in the polarization over unrelated intractable issues like immigration. It’s hard to get anything passed in a Congress that produced a record low 27 laws last year, including one law that created a commemorative coin and two laws that renamed medical centers, Anderson points out.
“It was the worst performance in the history of the country. The bickering really produced almost no real progress on any legislation. There’s just a lack of focus and, frankly, dysfunction, in Congress right now.”
He says NACDS, by contrast, is unified in the effort to call attention to the harm of PBMs’ direct and indirect remuneration (DIR) fees and other tactics. That was evident from the more than 300 pharmacy advocates knocking on the doors of senators and representatives last month for NACDS RxImpact Day, getting out the word on the need for reform.
With elections coming and drug prices being a top-of-mind issue, the easiest route to lower prices is the PBM bills, he notes. “So we’re continuing to put the heat on and do what needs to be done, both behind the scenes and out front as we did with the RxImpact news conference on the Hill.” That event featured pro-pharmacy messages from Senate Finance Committee chair Ron Wyden (D., Ore.) and ranking member Mike Crapo (R., Idaho).
Anderson says PBM reform enjoys broad bipartisan support in both houses of Congress. NACDS’ effort to educate legislators on the issue dates to 2011, and its “Too Big to Play Fair” campaign. The association has since made great progress in communicating the dire need for reform. “So everybody wants to help us out. It’s not a function of lack of support. It’s a lack of will to get anything done. We’re still plugging away. I’m hopeful we’ll get something, but I want to make sure we get what we want and get it done right. It’s a tough battle.”
The failure to enact a statute has not come from a lack of choices. A host of PBM reforms passed by the full House and key Senate committees last year includes the Lower Costs, More Transparency Act, the Pharmacy Benefit Manager Reform Act, the Modernizing and Ensuring PBM Accountability (MEPA) Act, and the Better Mental Health Care, Lower-Cost Drugs, and Extenders Act. The House Energy and Commerce Committee approved other PBM policies in December, including a policy to limit PBM income to nothing outside of flat dollar fees for the services provided for Medicare Part D drugs — a reform similar to that in the MEPA Act.
There’s also broad bipartisan support for provider status legislation called the Equitable Community Access to Pharmacist Services Act (H.R. 1770/S. 2477). Backing the bill is the Future of Pharmacy Care Coalition, which has NACDS on the executive committee and playing a leadership role. The coalition has made good progress, winning the support of more than 100 bipartisan members of the House, a dozen senators, and the endorsement of 200 organizations.
H.R. 1770 would ensure Medicare beneficiaries maintain prompt access to essential pharmacist services for the prevention, testing and treatment of common infectious diseases, including COVID-19, flu, respiratory syncytial virus (RSV), strep throat, pneumococcal and hepatitis B, and would create Medicare Part B direct reimbursement mechanisms for essential pharmacist services to protect seniors. H.R. 1770 is championed by Reps. Adrian Smith (R., Neb.), Brad Schneider (D., Ill.), Larry Bucshon (R., Ind.), and Doris Matsui (D., Calif.), and pharmacist members Earl “Buddy” Carter (R., Ga.) and Diana Harshbarger (R., Tenn.).
Morning Consult polls commissioned by NACDS have shown solid support for provider status from the public, which Anderson says is “an outgrowth of the incredible things that pharmacists and pharmacies did during COVID. The American people discovered — many for the first time — the services they were capable of providing. We’re leveraging that COVID response to push both provider status and a PBM bill.”
Outside of Congress, the Federal Trade Commission has been investigating PBMs for nearly two years. NACDS has been working with the FTC on the probe, says Anderson. He notes that Sen. Chuck Grassley (R., Iowa) sent a letter to the commission saying that PBMs were stonewalling the investigation at the same time they were killing the pharmacy industry.
Away from Washington, D.C., Anderson emphasized that some 150 PBM laws have been enacted in the states. The issue there is enforcement, because in many states PBMs have sued to block the statutes, despite the unanimous decision in the Supreme Court supporting such legislation in the 2020 Rutledge case.
Also on the state level, NACDS is working to secure the flexibilities and reimbursement mechanisms granted to pharmacists during the pandemic. The goal is to make permanent the authorities provided under the Public Readiness and Emergency Preparedness (PREP) Act. Anderson said that the association is urging states “to safeguard patient access by codifying swiftly at the state level all of the current federal PREP Act pharmacy-access amendments.”
Away from government, one focus of NACDS is its dedication to ending hunger and boosting nutrition. In January, NACDS joined policy makers, advocates, researchers and stakeholders at the Department of Health and Human Services’ first ever Food is Medicine Summit. Under discussion was the importance of the concept — and the ways in which pharmacies, other health care providers and stakeholders can work together to scale Food Is Medicine initiatives.
Anderson participated in a panel titled “Integrating Food is Medicine into Cross-Sector Systems to Advance Health.” He detailed the unique and powerful reach of pharmacies, including the industry’s integral role in delivering care to Americans during the COVID-19 pandemic. “Pharmacies gave tens of thousands of COVID tests for the American people … and more than 350 million COVID shots in a pharmacy setting. Estimates suggest pharmacies saved 1 million lives and that we saved the country $450 billion in health care costs. This illustrates how we can scale what we are doing with Food Is Medicine through our member company stores.”
After the pandemic, the NACDS board saw Food Is Medicine as a key means of boosting public health. “We listened to Americans,” said Anderson, citing Morning Consult polling that found 85% of adults in the U.S. say pharmacists are easy to access; 76% support pharmacists helping patients to understand their nutritional choices; and 73% support pharmacists helping patients prevent chronic disease such as heart disease and diabetes.”
In a related endeavor, NACDS has launched the Nourish My Health campaign as part of a commitment to the September 2022 White House Conference on Hunger, Nutrition, and Health. The campaign — which highlights the connection between food and wellness — is reaching millions of Americans, including those who live in underserved rural and inner-city communities. The initiative amplifies the importance of preventive screenings and raises awareness of the power of nutritious food as a part of lifestyle changes to improve health outcomes.
NACDS is partnering on Nourish My Health with the American Cancer Society, American Diabetes Association, American Heart Association, and the Food is Medicine Institute at the Friedman School of Nutrition Science and Policy at Tufts University. “It’s going very well,” Anderson says. “We’ve got great member engagement on it.”
The association was also prominent at February’s White House Challenge to End Hunger and Build Healthy Communities, making a new commitment to the Biden administration with the Milken Institute, which Anderson calls “the most prestigious public policy health think tank in the world.”
The new commitment outlines NACDS and the Milken Institute’s collaborative upcoming work to promote scalable implementation of accessible and sustainable Food Is Medicine interventions across diverse communities. The multiphase project is designed to identify needed policy changes for pharmacists to support interventions. It focuses on such undertakings as “food prescriptions,” and the possibilities of pharmacist compensation for such activities.
“The question is,” says Anderson, “should the accessibility of pharmacies be tapped to fill these gaps? And if you look at the Morning Consult polls, you see that most Americans feel that pharmacists can help them with their nutrition choices.”
He says the Milken partnership and Nourish My Health should be seen as part of a multipronged effort by NACDS to shape the future of retail pharmacy health care. The effort notably also includes supporting interoperability and technology advances for payment of services, which “is going to be crucial as we go from a fee-for-service health care system to a value-based system,” he notes. “We’re really focusing on the future — what retail health care is going to look like and how our members are going to get paid.”
Whatever the future brings, Anderson has confidence in the industry’s ability to thrive. “I tell people if they’re waiting for the government to aid their business, they probably shouldn’t bank on that — particularly in this environment. But I have great faith in the private sector, which has always been leading this country forward.
“There’s a lot that private companies can do, especially in an association like NACDS — because to do these great things in the future that we talk about, you can’t do them alone. You have to do it through an association where you have strength in numbers.”