PARSIPPANY, N.J. — Growth in spending on medicines dipped last year, but that hasn’t eased the challenge of balancing access to drugs and the cost of care in an era of innovative but more expensive treatments, according to the IMS Institute for Healthcare Informatics.
For the second year, medication spending climbed by double digits in 2015, reaching $425 billion, based on invoice prices, IMS said in its “Medicines Use and Spending in the U.S.” report, released Thursday. After adjusting for estimated rebates and other price concessions by manufacturers, net spending was $310 billion last year, up 8.5% over 2014 levels.
“So we’re reporting still relatively high levels of growth compared to what was seen since 2001, even as that growth has moderated off the 2014 levels,” Murray Aitken, executive director of the IMS Institute for Healthcare Informatics, said in a conference call on the report.
“We see that the surge of new medicines coming through the pipeline into the marketplace in 2014 continued into 2015. Demand for these newly launched brands remains high, certainly in the hepatitis C category but also in oncology, multiple scelerosis and other areas. We also saw in 2015 a relatively light year in terms of savings from branded medicines facing generic competition, although the savings were greater than in 2014,” Aitken said.
“We also saw a moderation in net price increases on branded drugs. That’s a reflection of higher rebates and price concessions by manufacturers as competition intensifies in many therapy areas — notably diabetes — and the negotiating power of pharmacy benefit managers and payers and the pressure on pricing has risen. The level of net price increases also reflects a growing contribution by manufacturers to patients in terms of copay coupons and vouchers to offset their out of pocket costs.”
Specialty drug spending swelled to $150 billion, up more than 20% from 2014, according to the IMS study. “We expect to continue to see robust levels of growth in spending on specialty drugs,” Aitken said.
Longer-term trends driven in part by the Affordable Care Act and in response to rising overall health care costs continued to play out in 2015. “The ACA’s provision for providing coverage to the uninsured through Medicaid expansion and health exchange plans have been the leading driver of retail prescription growth in the past two years,” the report stated.
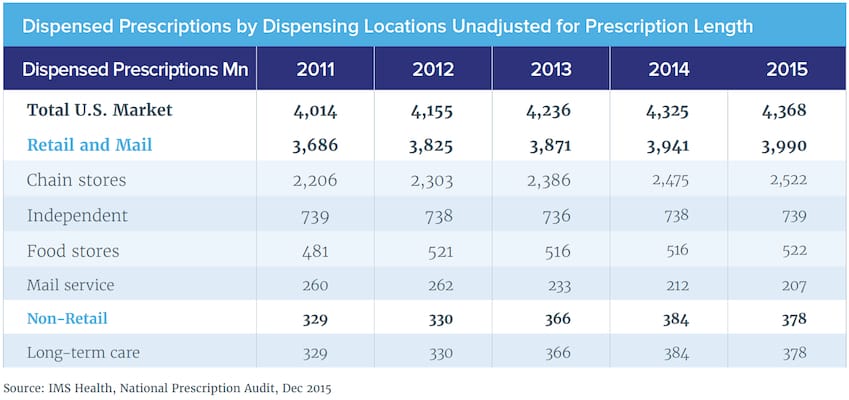
Prescriptions dispensed in 2015 totaled 4.37 billion, a gain of 1%, down from increases of about 2% in earlier years. Notably, mail-order prescriptions declined in 2015 as off-patent medicines were increasingly filled as generics at retail pharmacies rather than being managed through mail order.
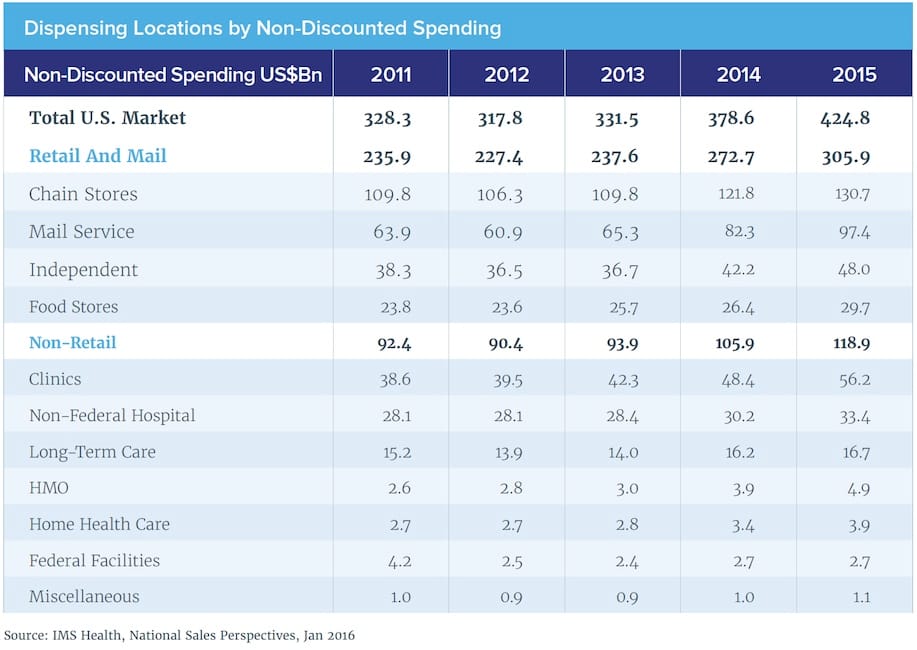
By channel, chain drug stores accounted for the largest share of prescription drug spending, with non-discounted expenditures rising 7.3% to $130.7 billion in 2015, IMS reported. That compared with $97.4 billion for mail service (+18.3%), $48 billion for independent pharmacies (+13.7%) and $29.7 billion (+12.5%) for supermarkets. Overall, non-discounted Rx spending — including clinics, long-term care, non-federal hospitals, HMOs, home health care, federal facilities and other providers — rose 12.2% to $424.8 billion in 2015.
In terms of dispensing (unadjusted for prescription length), chain drug stores totaled 2.522 billion prescriptions filled last year, a gain of 1.9%. By share in the retail and mail sector, that was followed by independent pharmacies at 739 million prescriptions dispensed (+0.1%), supermarkets at 522 million (+1.1%) and mail service at 207 million (-2.4%).
“Demand was higher in some therapy areas such as antidepressants and anti-diabetes, which registered about 10% increases, while other areas declined, including a notable 16.6% decline in the number of narcotic prescriptions dispensed,” the IMS study noted.
“The average patient cost exposure for a brand prescription filled through a commercial plan has increased by more than 25% since 2010, reaching $44 per prescription in 2015. Rising use of health plans with pharmacy deductibles, co-payments and co-insurance is contributing to this rise,” the report said. “The average patient cost exposure for generics, however, has remained at approximately $8 since 2010.”
In response to this rising level of patient cost exposure, branded drug makers are boosting their use of “buy-downs,” such as coupons or vouchers, to help patients offset these costs. In the diabetes market, for example, coupons are being used to reduce the patient cost exposure in commercial plans, in particular for patients facing $50 or more per prescription. Of those patients, about half were able to reduce their out-of-pocket cost to zero in 2015, IMS reported. Yet even after coupons are applied, patients with pharmacy deductible plans are still facing high cost exposure.
According to the study, over half of the total spending growth in 2015 was from new brands that have been available for less than 24 months. Patients are seeking and receiving new treatments for hepatitis, cancer, diabetes and other chronic conditions, driving $24.2 billion of new spending growth, slightly higher than in the year before and significantly higher than historical levels, IMS said.
Spending on all generic medicines contributed $7.9 billion to growth in 2015. Expenditures on branded generics — defined as non-original medicines marketed with trade names — rose sharply on an invoice price basis, though some of that may have been offset by price concessions, IMS pointed out.
Greater use of protected branded medicines contributed a modest $2.7 billion to growth in 2015, “but this is notable since in prior years, this element has had a negative impact on growth. The medicines contributing the most to volume growth were autoimmune and cancer treatments as well as anticoagulants,’’ the study said.
Medicines classified by IMS as “specialty” contributed $150.4 billion to the total spending on medicines in 2015, an increase of 21.6% over 2014. With more specialty treatment options becoming available and higher utilization, this segment remains one of the most dynamic of the total market, the report noted.
The surge of new treatments for patients with cancer continued in 2015 and contributed to rising expenditure on cancer therapeutics (excluding medicines used for supportive care), which reached $39.1 billion, up 18% from 2014.
Hepatitis C treatments that became available over the past two years were used to treat nearly 250,000 patients in 2015, up from 170,000 patients in 2014 and 20-30,000 per year in earlier periods. “However, the number of new patient starts moderated as the year progressed, suggesting progress in working through the initial group of patients with highest need,’’ the report said.
On an invoice price basis, spending on diabetes medications grew by $10.1 billion in 2015, totaling $43.9 billion. But IMS said that off-invoice price concessions of current and new brands stand to offset as much as $9 billion of that growth, particularly in the insulin segment.
Oncology drugs comprise the biggest share of launches by therapeutic area over the past 10 years, accounting for 35% of all launches in 2015, according to the report. A rising number of additional indications are being granted to existing cancer medicines, with 10 such approvals in 2015 in addition to the 14 indications given to newly approved drugs.
Among the launches of 2015 were notable advances in precision medicines, rare disease treatments, and chronic disease medicines that could benefit large populations.
“Significant advances occurred in 2015 for biosimilars, including the first approval under the biosimilar abbreviated pathway and subsequent launch, the submission to the FDA of seven biosimilar applications, and a growing number of biosimilar products advancing through clinical development,” IMS said in the report.
U.S. spending on medicines is forecast to reach $610 billion to $640 billion in 2020 on an invoice price basis, with steady mid-single digit growth driven by innovation and offset by loss of exclusivity.
Of the $282 billion of growth over the next five years from branded medicines, $91 billion is forecast to result from new medicines launched during that period, with the largest share coming from oncology, according to the study. Although brand price increases are expected to continue in the 10% to 12% range on an invoice basis, these will be significantly offset by rebates, discounts and other forms of price concessions, the report said.