Diabetes and prediabetes persist as widespread conditions, demanding care in their own right and threatening complications from eye problems to kidney disease. Pharmacists offer accessible care and education for the nearly 40 million Americans with diabetes and close to 100 million with prediabetes. In this virtual roundtable, retailers and suppliers discuss how pharmacists and the newest technologies can address the disease’s stubborn prevalence. Technologies and products can help stem nationwide increases in diabetes and prediabetes.
Panelists
JINALI DESAI
Vice President,
Pharmacy Health Services
CVS Health
SARAH FREEDMAN
Director,
Pharmacy Services Development
Walgreens
PHYLLIS HOUSTON
Vice President,
Pharmacy Enablement and
Performance
Good Neighbor Pharmacy
SUMMER KERLEY
Group Vice President,
Pharmacy Growth and
Clinical Programs
Rite Aid
SAMANTHA KETTERLING
Manager of Clinical Pharmacy
Thrifty White Pharmacy
NANCY LYONS
Chief Pharmacy Officer
Health Mart
CASEY PFLIEGER
Director of Retail Sales
Owen Mumford
CHERI SCHMIT
Senior Manager of Clinical
Programs
Cardinal Health
JEFF ZIVAN
Vice President,
Retail and Distribution
embecta
What are the latest ways pharmacies are addressing the persistence of type 2 diabetes and prediabetes?
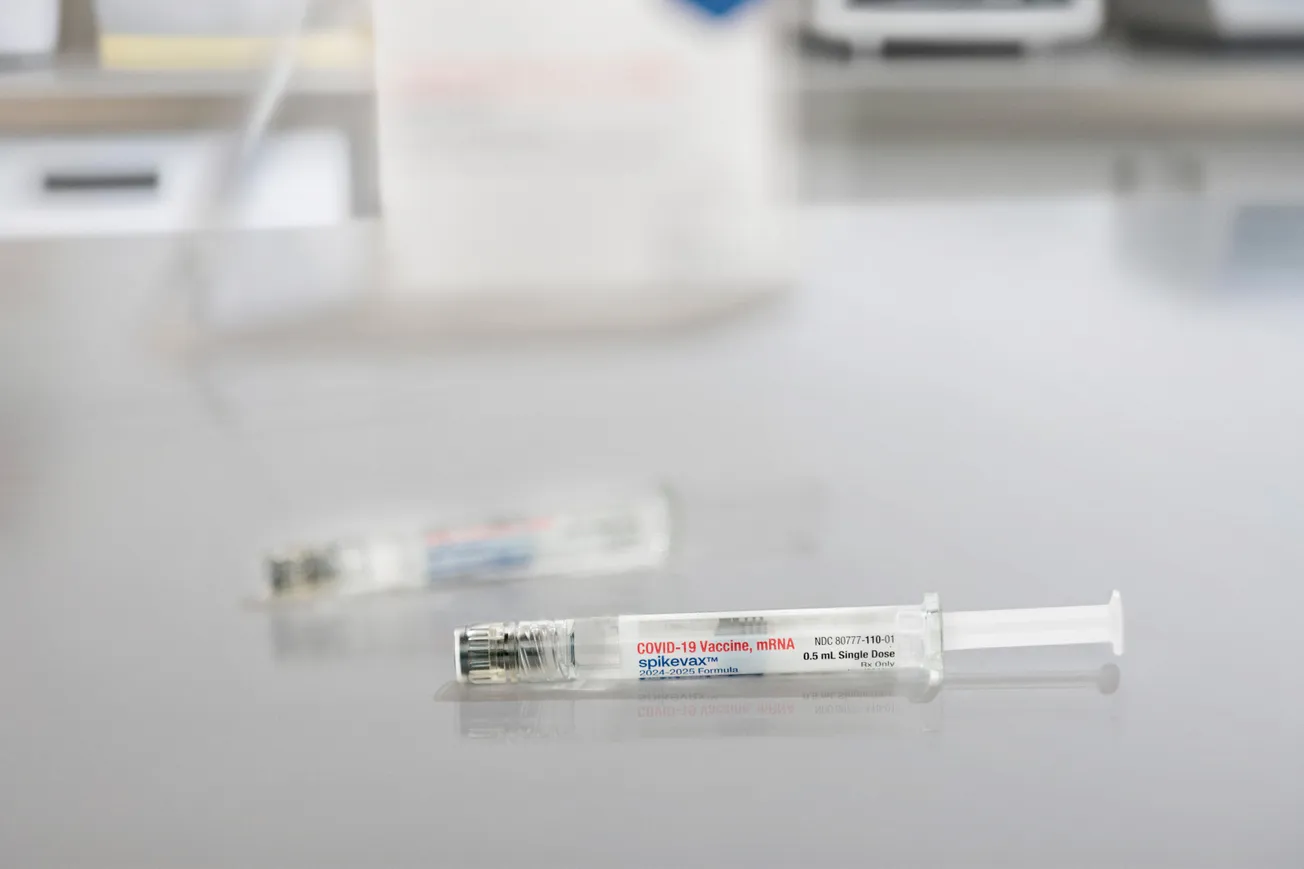
HOUSTON: Pharmacists are considered some of the most valuable and accessible healthcare representatives in their communities. Following the COVID-19 pandemic, pharmacists proved to be trusted resources to provide information and offer help with accessing COVID-19 tests and vaccinations. In addition to providing valuable expertise and guidance on prescriptions, pharmacists also serve as critical resources to patients on many health questions and concerns.
Patients are also looking for this extra support and guidance when struggling with diabetes risk or a diabetes diagnosis. Often filling a gap between patients and their doctors’ appointments, community pharmacies can really engage and educate on the importance of managing their conditions and helping patients adhere to their care plans.
With pharmacists, the opportunity for early identification and intervention in diabetes care is critical. This can include ongoing support with adherence to patients’ diabetic medications and glucose testing regimes, which are critical to diabetes care. It might also include education and best practices for pre-diabetes care to help prevent the eventual onset of type 2 diabetes, such as education about physical activity and a healthy diet to encourage weight loss. If patients do develop type 2 diabetes, pharmacists can provide important information to help with medication adherence and additional steps that patients can take proactively to maintain their health and help avoid complications associated with diabetes.

Summer Kerley, Group Vice President, Pharmacy Growth and Clinical Programs, Rite Aid
KERLEY: Historically, poor glycemic control is linked to nonadherence to medications, cost of medications, and complex treatment regimens. Pharmacists can address these barriers with adherence counseling and tools, reviewing the medication regimen for less costly alternatives or connecting the customer to manufacturer-sponsored savings programs, and addressing the complexity of regimens by looking for combination medications or providing patients with tools like phone apps or other reminders to help the customer stay on track with medications. This could entail:
- Medication adherence counseling/support
- Diabetes education
- Exercise, lifestyle, nutrition counseling
- Continuous glucose monitoring (CGM)
- Prevention
- Behavioral health approach
For prediabetes, providing the customer with education about the importance of dietary changes and exercise regimens, tailored to the customer is crucial.
FREEDMAN: As we continue to focus on holistic care for our patients, pharmacists are now providing a multitude of services to help patients manage their health, including new-to-therapy, medication therapy management and adherence consultations, barrier support, blood glucose and HbA1C screenings.
DESAI: We’re committed to being a trusted community health care resource, providing timely access to medications, medication and lifestyle counseling, and a wide array of products to support the care of those with diabetes (e.g., glucose meters, test strips, lancets, low sugar cough and cold products, etc.).
We’re also driving market leading adherence results for diabetes therapies and looking for ways to expand the role of the pharmacist to provide a greater degree of clinical support for diabetic patients.
ZIVAN: Pharmacists play a significant role in the care and comprehensive treatment of people with type 2 diabetes. From pre-diabetes screenings and point-of-care testing, to focusing on stronger adherence to their diabetes treatments, pharmacists know the combination of education, counseling, and innovative products that can help their patients improve their diabetes management.
Embecta continues to look for ways to collaborate with our retailers to help with patient engagement programs and tools they need to improve adherence. Additionally, embecta is focused on broadening our insurance coverage so all patients can have access to the products they want. embecta pen needles and insulin syringes are covered by most health plans across Commercial, Medicaid, and Medicare Part D.
Cheri Schmit, Senior Manager of Clinical Programs, Cardinal Health
SCHMIT: The role of the pharmacist in diabetes care has evolved from providing traditional services, such as medication counseling, adherence, disease state education, and glucose monitoring, to more complex services, such as diabetes prevention programs, diabetes self-management education and chronic disease management, including remote patient monitoring.
As one of the most accessible, convenient, trusted and knowledgeable healthcare providers, pharmacies are playing a larger role in the health of the patients they serve. They often act as an entry point to care, helping screen and refer patients to other providers and to navigate the often complex and confusing healthcare system.
According to the National Association of Community Health Centers, an estimated 100 million U.S. patients do not have a primary care provider (PCP). Pharmacists can help close this gap by screening, identifying, and referring patients at risk or with early onset symptoms to providers. In the absence of a PCP, pharmacists are addressing basic needs for these patients, including education, screening, immunizations, over-the-counter consults, medication reconciliation, and improving adherence through medication synchronization and compliance packaging.
They are also addressing social determinants of health, helping patients connect to community resources to address and solve health inequities such as access to healthy food, affordability of medications, transportation, health literacy and more.
In addition, pharmacists are helping improve quality metrics and close gaps in care by educating patients with diabetes on the need for a statin and making sure patients are up to date on routine immunizations for flu, pneumonia, shingles and tetanus, diphtheria and acellular pertussis (Td or Tdap).
Patients exceedingly rely on and expect a broader more complex range of services from their pharmacy, and pharmacies are adapting to fill this need as a healthcare destination, providing greater value and helping to drive improved outcomes.
PFLIEGER: Medication adherence is one of the biggest challenges with T2D, and is critical for slowing disease progression and improving glycemic control, ultimately preventing diabetes associated complications and lowering the risk of hospitalization and mortality. Pharmacies have been very successful in the implementation of Med Sync programs to drive medication adherence, and execution of these programs has a financial upside for the pharmacy as well, assuming the pharmacy is reimbursed favorably for the drug being dispensed.
Unfortunately, with the majority of T2D patients falling under Medicare, declining reimbursement rates for Part D have put many independent pharmacies in an uncomfortable position, where they are underwater on critical medications—in some cases forcing them to turn away patients because they simply can’t afford to serve them. The watch-out here is that if this is allowed to persist, Med Sync has the potential to backfire. In a scenario where diabetes medications are not reimbursing high enough to cover operational costs, a pharmacy could be financially disincentivized to take on seniors living with diabetes, with many Rx refills serving another punishing blow to their bottom line. Progress could stall, or even reverse.
The topic of CMS and Medicare reimbursement is a sticky one, yet it can’t be ignored because it will drive decisions and significant change within the space. Declining reimbursement rates and formulary restrictions are making Medicare patients less attractive to pharmacies. This could push some pharmacies to abandon Medicare patients altogether, or for those willing to think outside-of-the-pillbox, this presents an interesting opportunity to capitalize on this customer if they are willing to explore Medicare reimbursed service offerings. While the drug reimbursement landscape is in flux, I’d be hedging my bets on leveraging billable service offerings. It turns out you don’t need “prescriber status” in all cases.
LYONS: Pharmacies play a critical role in public health, serving as the front door to healthcare. Embedded in their communities and equipped with the skills required, pharmacists are in a solid position to reach more people with or at risk for diabetes screening and referrals for earlier diagnosis. Following diagnosis, pharmacists can help improve outcomes through evidence-based self-care education, support medication management and adherence, and collaboration with other members of the patient-centered health care team to create individualized treatment plans patients can afford.
Health Mart, McKesson’s network of independently owned pharmacies, is perfectly positioned to support diabetes prevention and management as nearly 60% of Health Mart locations are located in underserved communities. To provide greater access to diabetes education, Health Mart formed a new relationship with the APhA Foundation, a Centers for Disease Control and Prevention (CDC) recognized umbrella hub organization (UHO) leveraging the power of Health Mart Atlas, McKesson’s Pharmacy Services Administrative Organization (PSAO). This relationship allows Health Mart and Health Mart Atlas members to enroll with a Centers for Medicare & Medicaid Services (CMS) Medicare Diabetes Prevention Program (DPP) supplier. The DPP curriculum is designed to help patients make meaningful lifestyle changes, achieve weight loss and better health.
Beyond supporting patients in achieving better outcomes, the program can enrich the career path for pharmacy technicians. As part of the DPP curriculum, pharmacies designate a member of their staff—usually a pharmacy technician—to complete lifestyle coach training and coordinate the program. This role is vital to helping ensure patient engagement with the curriculum and can refer patients to additional pharmacist-provided services. Member pharmacies that complete the participation criteria as well as provide and document the standardized patient education program requirements can receive CMS billing and payments through a streamlined process.

Samantha Ketterling, Manager of Clinical Pharmacy, Thrifty White Pharmacy
KETTERLING: Integrating pharmacist involvement in diabetes care management, as well as further patient engagement with pharmacist provided care, has helped influence diabetic and prediabetes clinical outcomes. Focused efforts including diabetes disease management programs, addressing social determinants of health and assisting with coordinating care across the healthcare system has helped address the persistence and the persistence of type 2 diabetes and prediabetes.
To what extent would elevated provider status help pharmacists in that effort?
FREEDMAN: As an industry, we need to continually focus on regulatory advancements such as nationwide provider status to allow pharmacists to perform more diagnostic screenings, deliver results and provide comprehensive medication management services, all while ensuring appropriate compensation.
As integral members of the healthcare team, pharmacists with provider status could bill medical insurance for clinical services rendered. Adjacent regulatory pushes would allow pharmacists to perform diagnostic screenings such as A1C and blood glucose test and provide results of those tests, as well as engage in more Collaborative Practice Agreements for comprehensive diabetes management services.
Research has shown that pharmacists make a tremendous positive impact on health outcomes for patients with diabetes, improving efficiency and reducing overall healthcare cost. Obtaining provider status for pharmacists would offer expanded access to crucial care for many underserved patient populations in need of health care.
KETTERLING: Elevated provider status would help pharmacists manage patients with type 2 diabetes and prediabetes by expanding the degree of intervention they can provide for a particular issue. Pharmacists do an excellent job collecting, assessing and making a care plan to intervene and improve outcomes for diabetic patients. However, the rate limiting step is often during implementation. Today, changes to drug regimens including dose optimization, alternative therapy, additional therapy, and social or medical resources require a new prescription from a medical provider or a referral for additional care. Recommendations and referrals do not always reach the provider to be addressed. Elevated provider status would allow pharmacists more opportunity to implement the care plan they came up with by having authority to make changes, additions or substitutions to their therapy.
PFLIEGER: Would provider status help lessen the blow of declining Medicare Part D reimbursement? Absolutely. However, policies take time, and for many pharmacies who are already struggling to make ends meet, time is not on their side. Rather than crossing one’s fingers and waiting, I’d look at what exists today and see if there are ways to take advantage of these programs. The CDC recently released their new “Diabetes Self-Management Education and Support Medical Billing Playbook for Pharmacies,” where they define a roadmap for obtaining pharmacy reimbursement in exchange for providing the critical diabetes educational services that our seniors need. I’m sure the process isn’t perfect, but it’s a starting point and a path forward that acknowledges the unique ability pharmacies have to reach and engage with patients living with diabetes.
SCHMIT: Expanding provider status would be a game changer for pharmacists. Pharmacists today are providing a number of clinical services without being recognized as a provider by a patient’s insurance plan and therefore cannot bill for the valuable services provided. Currently, there is no nationwide provider status legislation, meaning that a pharmacist’s ability to bill payers and be reimbursed for their services varies not only from plan to plan but from state to state as well.
Despite this added complexity, resourceful, resilient pharmacists continue to put the needs of their patient first, finding innovative ways to partner with public health or other community resources, find grants, and establish wellness programs with employers, among other approaches.
Some pharmacists are able to bill specific insurance plans for specific services; and of course, they have cash-pay programs for those that can afford to pay. They may even provide services free of charge because the patient needs it.
The ability to bill all types of insurance plans for all services provided within scope would be revolutionary. Not only would expanded provider status allow pharmacies to create a revenue stream to help ensure they can continue to serve their communities particularly in rural or underserved “pharmacy deserts” where access to care is limited, it would also help reduce the strain on the healthcare system by allowing pharmacists to provide lower level services within scope, improving patient access, health and outcomes.

Nancy Lyons, Chief Pharmacy Officer, Health Mart
LYONS: Provider status is critical to the future of the pharmacy profession and the overall sustainability of patient care resources. Many states have enacted laws that grant patients access to an expanding range of healthcare services provided by pharmacists. These services, which are often delivered as part of cost-effective, team-based care, can include diabetes screening, education, and treatment adherence programs, along with other non-diabetes related services such as vaccinations. However, the lack of Medicare Part B coverage for pharmacist-provided services creates barriers to care for vulnerable community members.
McKesson is a strong advocate for the elevation and long-term success of the pharmacy profession, dedicated to ensuring that pharmacists nationwide can continue delivering critical services to patients. As part of the Future of Pharmacy Care Coalition, McKesson and Health Mart actively support H.R. 1770 and S. 2477, the Equitable Community Access to Pharmacist Services Act. This legislation aims to establish federal reimbursement for pharmacist services under Medicare Part B, removing financial barriers and enabling continued access to essential services. Until this happens, pharmacies will continue to spend time and resources to find ways to receive reimbursement for the services provided, taking time away from patient care.
HOUSTON: Increased point of care testing and screening would help pharmacists continue to address the prevalence of type 2 diabetes and prediabetes. For this to happen, pharmacists across the country will need to have the expanded ability to order tests and interpret lab results related to diabetes management, as well as the authority to potentially adjust or make recommendations about treatment regimens in coordination and collaboration with patients’ healthcare providers.
With this expanded ability, pharmacists would be able to provide screenings for A1Cs (a critical measure of blood sugar control), cholesterol and blood pressure, and then collaborate closely with other healthcare providers to help patients adjust their treatment regime. The more frequently a patient’s glucose, blood pressure and blood lipids are monitored is ideal for optimal patient health. Therefore, increasing the ability of pharmacists to provide screenings through a point of care testing method allows for a more accessible point of contact for a patient.
In addition, there’s value in pharmacists being close to patients’ medical records. This gives pharmacists the ability to recognize gaps in care quickly and recommend other health exams a patient may be missing such as regular ear and eye health checkups, and then coordinate with other specialists and healthcare providers.

Jinali Desai, Vice President, Pharmacy Health Services, CVS Health
DESAI: Provider status would further enable pharmacists to offer services within their clinical ability and state scope of practice while facilitating patient coverage for the service; pharmacists have a broad set of clinical skills they bring to the care team, but more needs to ensure patients are covered to receive that care.
Provider status would help make expanded services sustainable as pharmacists play a greater role in chronic condition management and fill the expected gap in primary care services, especially in underserved communities.
Provider status for pharmacists is primarily hindered by a lack of federal authority that would recognizes pharmacists with covered provider status, in line with other health care practitioners.
KERLEY: Elevated prescriber status would allow pharmacists to practice at the top of their licenses by allowing them the ability to adjust medication regimens for chronic conditions such as diabetes and hypertension, complete point-of-care testing for hyperlipidemia, and monitor blood glucose or blood pressure. The elevated provider status could allow for billing for these services to insurance while allowing customers convenient access to care. It would mean:
- Better access to care
- Enhanced Medication Management – optimizing pharmacy programs to support adherence
- Integrated Care
- Expanded Scope of Practice = Improved patient outcomes
ZIVAN: When it comes to ensuring people with diabetes are properly managing their A1C, elevated provider status can enable pharmacists to oversee their patients’ treatment plan and optimize their medication therapy, alongside other physicians and healthcare providers. With certain provider status, pharmacists may be able to initiate and adjust diabetes medications, including insulin, based on certain patient criteria, allowing for expanded scope of practice. Pharmacists have the ability to support better health outcomes for insulin-dependent patients by educating them on the importance of proper injection technique training, having an adequate needle supply, and recommending appropriate injection products (i.e., a 4mm pen needle with features such as a contoured needle base) to improve their injection experience. Elevated provider status enables pharmacists to take on a more proactive and involved role in patients’ diabetes care, potentially leading to better diabetes management for individuals living with diabetes.
How effective have existing approaches been and what have been the headwinds and tailwinds?
KERLEY: A systematic review by Al Assaf, et. al. in 2022 demonstrated significant increases in medication adherence and better glycemic control in response to adherence and self-management support counseling as well as medication therapy management conducted by pharmacists. Barriers on the part of pharmacist provision of services include lack of time, training, and resources; public awareness; and collaborative arrangements with other healthcare professionals.

Jeff Zivan, Vice President, Retail and Distribution, embecta
ZIVAN: Counseling programs with pharmacists can optimize medication use outcomes and may drive adherence to therapy. Several studies reported that patients with poorer glycemic control at baseline obtained greater benefits from pharmacist intervention, including improved A1C levels. Furthermore, studies assessing patient quality of life (QOL) found that pharmacist-managed diabetes care initiatives demonstrated improved QOL measures, including patient satisfaction.
Other studies show that injection technique training may help improve diabetes management.4 For example, people with diabetes on insulin who received proper injection technique training, including using a new needle for every injection, rotating injection sites, and moving to a shorter 4mm or 5mm needle, experienced up to a 1% reduction in A1C at 6 months.
Although pharmacists can have a positive impact on patient health outcomes through individualized counseling sessions, staffing shortages and high prescription volumes within community pharmacies can make it challenging to implement effective counseling programs to further optimize diabetes care. However, with the addition of call center pharmacists, digital tools, and pharmacy system enhancements, there may be opportunities to overcome these challenges and support efficient counseling sessions.
LYONS: Bipartisan support has increased for current provider status bills in both the US House of Representatives and the Senate. Aside from that critical work on the national level to modify title XVIII of the Social Security Act, a growing number of payers recognize the value in pharmacist-provided patient care and have set up alternate processes. However, these alternate processes can create billing complexity, straining the sustainability of the service for many providers.
On the patient care side, existing approaches for pharmacies to address the persistence of type 2 diabetes and prediabetes have produced mixed results. While pharmacists have the knowledge, skills and medications, patients experience multiple barriers that can require additional education and interventions. Personal motivations, time and resources, along with out-of-pocket costs of medications are all factors in achieving desired outcomes. Some of the newest, most effective treatments have high costs that impact adherence, yet more affordable options present tradeoffs that are difficult to manage.
As an industry, we must continue to focus on the development and commercialization of innovative new treatments, double down on education and prevention, and push for legislative solutions to achieve realistic costs and reimbursement for all medications, supplies and up-to-date monitoring technologies related to prevention and treatment.
KETTERLING: Existing approaches towards provider status have included state legislation changes including drug specific prescriptive authority, expanded collaborative practice agreements and pharmacist credentialing status. Some state programs have moved towards recognizing pharmacist’s as providers of which they are the rendering providers when billing clinical services, such as Medication Therapy Management. These approaches have been effective to increase engagement from patients, pharmacists and providers. The challenge is that these are not consistent across all states or health plans.

Casey Pflieger, Director of Retail Sales, Owen Mumford
PFLIEGER: Recently I ran across a statistic that surprised me. Since 2008 the incidence of newly diagnosed diabetes cases in America has been declining. According to the CDC’s National Diabetes Statistics Report, newly diagnosed cases declined between 2008 (8.4 per 1,000 adults) and 2021 (5.8 per 1,000 adults). This suggests that the combined efforts of healthcare professionals, diabetes associations and pharmacies to emphasize the important role of weight management, healthy eating and exercise on disease prevention is likely having an impact. Eventually with the growing use of GLP-1s for weight management I imagine we could see further improvements, assuming coverage gaps are fully addressing making these medications more accessible.
If newly diagnosed cases are declining, how is it possible that the number of people living with diabetes continues to increase? As therapies have advanced, medication adherence has improved and people have begun making healthier lifestyle choices, we are seeing people with diabetes live longer lives.
For the pharmacy this bears significance because it equates to a higher percentage of these patients falling under Medicare, with many being served in LTC pharmacy in addition to traditional retail pharmacy. Here again, reimbursement challenges and formulary decisions that impact Medicare will have a lasting effect. From Medicare drug pricing to PBM reform bills, the stakes are high, the players are numerous, and no one knows yet how the dice will roll. The only thing for certain is that we will continue to have more and more T2D Medicare patients. How pharmacies balance patient wellness with the health and sustainability of their business remains to be seen.
A growing senior and geriatric population also suggests that we should be paying closer attention to LTC pharmacy, and that it will become increasingly important for pharmacists to broaden their knowledge base to understand the unique challenges medically complex seniors represent. I would expect demand for Consultant Pharmacists to increase significantly over the coming years, and that we will see further diversification and evolution of the retail pharmacy business model to embrace LTC and clinical service offerings.
SCHMIT: The effectiveness of existing approaches to diabetes management have varied from pharmacy to pharmacy and state to state because of a lack of consistency as to the scope of provider status, Because of this, the full scope of what a pharmacist can do to support diabetes patients in their community is not being realized. Additionally, the inconsistency between credentialing and contracting requirements for medical billing also varies from insurer to insurer, adding further complexity and reducing the effectiveness of existing approaches to helping patients manage their diabetes.
Pharmacies are proficient in billing a patient’s pharmacy benefit, but most are unfamiliar with medical benefit billing. Better documentation platforms, more access to EHRs and greater connectivity to other providers is needed for pharmacists to fully realize their potential on a patient’s care team.
The current reimbursement headwinds have forced many pharmacies to make staff and operational cuts; and of course, pharmacy is not immune to general workforce issues of labor shortages, increased wages and cost of staff, staff training, retention, etc. Most pharmacies are trying to do more with less, which makes it difficult to offer services without reimbursement or sustainability.
The opportunity to step up for their communities as part of the vaccine delivery network during the COVID-19 pandemic was a tailwind for pharmacies because it demonstrated the value of pharmacies as community healthcare destinations. As such, patient demand for access to clinical pharmacy services has increased. This is evidenced by a Wolters Kluwer Pharmacy Next survey that showed nearly 60% of Americans are likely to visit a local pharmacy as their first point of contact for treating non-emergency health issues. The National Association of Chain Drug Stores (NACDS) recently published data that shows more than 80% of patients want to ensure continued access to vaccination, testing and treatment services they accessed through their local pharmacy during COVID-19. Within the next five years, more than half of patients anticipate visiting pharmacies, retail clinics or pharmacy clinics for the majority of their primary care services, according to Wolters Kluwer.

Phyllis Houston, Vice President, Pharmacy Enablement and Performance, Good Neighbor Pharmacy
HOUSTON: From a headwinds perspective, while current approaches make a difference for patients, they’re not consistent. State boards have different regulations when it comes to the pharmacy’s scope of practice. This is why the federal provider status is so critical.
Provider statutes make it easier for patients to understand the role that pharmacists can play, especially when it comes to disease management. Another headwind is creating a robust reimbursement model that aligns with the scope of practice. Pharmacists must be paid for the additional services they perform under their expanded scope of practice.
In terms of tailwinds, it’s the ever-evolving solutions in the market. We are seeing more and more solutions and technology come to bear to support patients. We know that adherence is a key component, and pharmacies continue to focus on this. Medication non-adherence has detrimental implications for patients and their quality of life and also has an impact on pharmacies. With real patient healthcare value at stake, managing medication adherence is critical for independent pharmacies.
Thankfully, there’s many ways that pharmacies can improve patient medication adherence. One way includes identifying patients that could benefit from a medication synchronization program. Medication synchronization is the coordination of all medication refills for patients to pick up at the same time each month. This ensures a lack of interruptions in therapies and provides a better overall experience for patients—no more walking out with missing scripts or partial fills. Successful programs can help patients stay adherent and increase pharmacy business efficiency.
We can also look to front-end products to round out solutions for diabetic patients. It’s important for pharmacists to remind patients that they can turn to their pharmacy for diabetic testing supplies and other products that support their overall health. The pharmacy is truly a one stop shop right in patients’ backyards for everything they need to manage their condition.

Sarah Freedman, Director, Pharmacy Services Development, Walgreens
FREEDMAN: While some strides have been made to offer diabetes care services within the community pharmacy setting, challenges such as cost of implementation and maintenance of new clinical services, continued reimbursement struggles in addition to limited community awareness and uptake of these extended clinical service offerings have impeded more robust progress.
Nevertheless, the immense response of community pharmacists and their critical roles in managing the COVID-19 pandemic have highlighted the pharmacists’ extensive capabilities beyond medication dispensing and brought awareness to their key public health role. With the pharmacy being one of the most accessible healthcare locations — along with increased awareness and acceptance of services provided by pharmacy — now, more than ever, the pharmacy is being recognized as a key player in the healthcare ecosystem.
How can suppliers help in the effort?
ZIVAN: Suppliers can help support patient counseling by providing educational content, such as videos, brochures, fact sheets, and other resources that pharmacists can distribute, as needed, to their patients to take home. These resources may help facilitate productive discussions with patients about their medication therapy and may help support better diabetes management.
Suppliers have an opportunity to raise awareness of improving diabetes self-care. For example, embecta is investing in an unbranded campaign, delivered through an omnichannel approach, to help educate both pharmacists and patients on the importance of proper injection technique and having sufficient pen needle supplies.
PFLIEGER: Suppliers have many responsibilities and ways that they can assist customers in helping manage diabetes patients. Fundamentally it is our responsibility to help ensure continuous supply and market access for our products. While this may sound simple, we are only one part of a highly complex supply chain. Communication is important between our pharmacy customers, our account managers, our buying group partners and our distributors. Without those relationships and communication, the system is subject to failure. In a healthcare system where people’s health and lives are at risk, I see failure as unacceptable, and yet we’ve seen many supply failures over the past several years from various healthcare companies and points within the supply chain. Owen Mumford’s National Account Manager team does a phenomenal job communicating between our stakeholders to help make sure our products are ready and available for our pharmacies and the patients that need them. We’ve managed to remain a reliable, consistent supplier based on this steady communication and the combined strength of our operations, production, customer service and regulatory teams. Additionally, as a UK based manufacturer with US packaging facilities we are able to achieve flexibilities to respond to changing customer and market demands under shorter lead times.
Additionally, we provide marketing, educational and sampling support for our partners. Many take advantage of our complimentary Insulin Injection Guides, which offer step-by-step guidance for pen needle users to discourage reuse and encourage site rotation.
From a product development perspective, Owen Mumford is also unique in our approach. When we develop products, we look for ways to address unmet needs in market, which often means making products safer, easier and more convenient for patients. When you make products that patients find easier to use, they tend to use them more often and compliance is an added benefit.
KETTERLING: Continued collaboration between pharmacies and suppliers on varying diabetes and education programs to support pharmacist’s accessibility and patient’s trust including will remain helpful. This includes diabetes support programs, resources for new start education, adherence monitoring, and therapy optimization options.
Additionally, increased education and resources from insulin manufactures on approved biosimilars and cost-saving alternatives for pharmacies has been useful in our practice.
HOUSTON: Suppliers can help provide a broad range of medication supplies and products that help patients take a more active role in their health and better control of their disease state. Cencora works with numerous suppliers to offer a comprehensive range of diabetes products tailored for our pharmacy customers, so they can better serve this patient population. One specific example of these products is diabetic shoes or inserts, which help patients reduce the risk of foot ulcers and improve mobility. Custom shoe fittings are just one more way pharmacists can support diabetic patients in their community.
Good Neighbor Pharmacy provides the resources and support to help customers optimize their use of these supplies and successfully manage diabetes care management programs within their pharmacies. Our experts are available to work one on one with customers to streamline the process and implementation of their programs every step of the way. Additionally, we recently launched a resource section on Good Neighbor Pharmacy University (our e-learning platform available to all Good Neighbor Pharmacy and Elevate members) about diabetes care and how pharmacies can more efficiently step into this space to treat their diabetic patients.
DESAI: Suppliers can help ensure continuity in medications through smooth supply and distribution to help drive adherence.
SCHMIT: Pharmacies need flexible, dynamic partners to help them evolve and scale to a sustainable model. Cardinal Health understands the challenges and opportunities pharmacists are facing and is passionate about the importance of pharmacies to the communities they serve. We are centered on support for pharmacies by providing the financial, business, operational and clinical solutions they need now to evolve as a community healthcare destination and into the future to ensure their success. We are advocating for change in the industry, working alongside industry organizations to champion provider status and promote the valuable role of the pharmacist in healthcare. We listen to our customers’ pain points and work to provide solutions to address their needs and concerns.
KERLEY: Suppliers can help mitigate shortages of medications for diabetes and provide price reduction strategies to ensure continued customer access to equitable pricing for necessary medications. Additionally, manufacturers can provide the following:
- Essential resources, tools, and partnerships/collaborations
- Product Research and Development investments (diabetes products, medications, devices, and technologies)
- Education and Training
- Data on utilization patterns, patient adherence, prescribing trends
What new technologies, beyond CGM, can make diabetes management easier and more productive?
DESAI: There are a variety of digital innovations that can play a role in diabetes management, specifically in pharmacy, such as connected smartpens that allow patients to activity track and monitor their insulin doses and continuous glucose monitors (CGMs) that let patients monitor their blood glucose levels in real time to reinforce lifestyle improvements.
KETTERLING: The value of real-time monitoring and accurate reporting to influence therapy optimization has been better realized by prescribers, pharmacists and patients. Further development of Remote Patient Monitoring services and Telehealth services, including program implementation, specifically in pharmacies, holds great opportunity for pharmacists to play an integrate role on the patient’s health care team for chronic diabetes management.
Expanded healthcare technology, interoperability and streamlined referral process between pharmacies and Primary Care Providers/health systems/healthcare resources will continue to bridge the gap between care providers and allow for diabetes care optimization and improvement in clinical outcomes.
All of which provide pharmacists with additional resources to better manage diabetic patients beyond what they can utilize from dispensing systems.
FREEDMAN: Over the years innovative technological advancements have expanded diabetes treatment options. In addition to continuous glucose monitoring (CGM), improvements in smart insulin pens, insulin pumps, automated insulin delivery (AID) systems that combine insulin pump and CGM technology, and diabetes self-management support software continue to transform the way we treat diabetes.
Diabetes technology can reduce the burden of diabetes and provide patients with flexibility, empowerment, improved self-management and an enhanced quality of life. In addition, it can improve patient-provider engagement and positively contribute to more informed, personalized data-driven treatment recommendations that optimally improve patient care and diabetes management.
ZIVAN: New insulin pumps, smart insulin pens, and smartphone applications are just a few newer technologies that can support diabetes management. These technologies can help patients better track their dose of medication, provide helpful reminders/alerts, make decisions about medication dosing, provide nutrition support, and equip them with other useful tools to help them navigate their diabetes care journey.
Earlier this year, embecta submitted a 510(k) premarket filing to the U.S. Food and Drug Administration (FDA) for a proprietary disposable insulin delivery system. This patch pump is intended for people who require insulin to manage diabetes and is designed to be a simple and convenient option for automated insulin delivery with ease of use and discretion of a patch pump, along with a large 300U insulin reservoir. The 510(k) submission of our patch pump to the FDA is an important step in the advancement of our strategic priorities, and we believe has the potential to positively impact diabetes management for many people. embecta continues to advance its patch pump development program, with plans for a closed-loop version including an insulin-dosing algorithm, in a future FDA submission.
Pharmacists can play a valuable role in the treatment of people with diabetes by leveraging these new technologies and further building long-standing trust and reliability with their patients.
PFLIEGER: When it comes to diabetes care, anything that makes medication management easier or more convenient can help improve outcomes. As long as products are stocked and available through wholesalers, while also being covered under most insurance plans, they will be capable of having a positive impact on patient adherence and quality of life.
At Owen Mumford, our Unifine Pentips Plus pen needles are a great example of this. These pen needles offer the added convenience of a pen needle remover built into the disposable outer hub, which helps to make it easier for patients to change their pen needles. In an observational behavioral study this had a positive impact on patient adherence, resulting in a 61% increase in patient compliance. With many T2D also facing dexterity loss, the product is also easier to handle and grip.
As seniors and the geriatric population continue to make up a disproportionately larger part of the diabetic community, it is important to also consider the unique needs of the LTC facilities. In most instances these facilities use safety pen needles, and here again, Owen Mumford offers an innovative solution. Our Unifine SafeControl safety pen needle is designed to overcome the drug delivery challenges experienced with passive safety devices in market. Unlike passive devices where the needle can accidentally lock-out prematurely or fail to penetrate adequately, Unifine SafeControl puts control in the hands of the user. The user activates the safety after they are fully confident the dose has been delivered, providing greater confidence, reassurance and control.
KERLEY: Diabetes technology combined with education and support, can improve the quality of life and health of people with diabetes; however, these tools are sometimes complex, and can also be a barrier to acceptance and therapy initiation for people with diabetes and their caregivers. Pharmacists can provide counseling and guidance to ensure better medication therapy outcomes. Pharmacists utilize their clinical expertise to educate customers and empower them to take an active role in managing their health.
Technologies include: smart insulin pens, patch pumps and closed-loop insulin delivery/artificial pancreas, remote monitoring, Telehealth/telemedicine, and smartphone apps.
LYONS: Continuous glucose monitoring (CGM) devices are truly a game changer in the management of diabetes, especially with advancements in technologies and coverage for more patients. The glucose trending indicators, alarms and other features make them an easy solution to maintain control with fewer fingersticks required.
CGMs, smart insulin pens and other new technologies allow pharmacists to get a more complete picture when making medication adjustments recommendations. Additionally, smart phone applications that help describe carbohydrate, calorie, and glycemic index can support adherence. Ultimately, any technology that makes it easier for patients to manage complicated tasks such as insulin dose calculations, can contribute to better outcomes and lessen the burden of the disease and improve the patient’s quality of life.
How have insulin price reductions, and competition from biosimilars, affected management of type 1 diabetes and insulin-dependent type 2?
KETTERLING: Insulin price cuts and the approval insulin biosimilars have led to increased patient access to insulin therapy, decreased the frequency of patients rationing their supply and has allowed for appropriate prescribing habits and escalation of therapy if indicated for patients. Public awareness of the more affordable options amongst patients, providers and pharmacists helps mitigate cost as a barrier to appropriate diabetic therapy and in turn we should anticipate more diabetic patients making progress towards meeting their goals of therapy.
FREEDMAN: Diabetes takes a tremendous toll on Americans, physically and economically. Patients with type 1 diabetes and numerous patients with type 2 diabetes rely on insulin to manage their diabetes. Lack of access to affordable insulin is a barrier to care and adherence for many, especially those with lower incomes or high-deductible health plans.
While there is no simple solution, insulin price reductions and the continued introduction of more potentially cheaper biosimilar insulin products support efforts to provide access to more affordable diabetes care. Access to insulin therapy helps eliminate some barriers to proper diabetes management, which optimally over time can improve our patient health outcomes and reduce the overall financial and operational burden on the health care system.
SCHMIT: Price reductions and competition from biosimilars have helped make medication more affordable for some patients; however, the individual patient’s insurance plan and formulary may impact the savings to that patient. Additionally, new entrants to the diabetes market, such as GLP-1s, may help patients better manage their diabetes, but they are costly and there have been supply constraints due to demand.
Diabetes is a complex, progressive and expensive condition with insulin being just one facet of treatment. The highest standard of care would also include frequent testing to monitor and inform, along with lifestyle changes such as a healthy diet and exercise. Many patients struggle to be able to afford testing and supplies, other medications that go along with the treatment of diabetes, healthy food, and copays for provider visits and care.
KERLEY: Insulin price reductions and biosimilars have provided more affordable options and improved access to insulin for customers who require this medication. Eliminating cost barriers improves medication adherence and therefore glycemic control.
ZIVAN: High insulin prices can be a barrier for people with diabetes, which may lead to rationing or skipping doses and potentially lead to serious health complications. Insulin price reductions and biosimilars may provide better affordability and access to the medication, allowing more people to properly manage their diabetes.
With better affordability and access to insulin, people with diabetes may be more adherent to their therapy, leading to better blood glucose control and overall health outcomes. This can reduce the risk of long-term complications associated with diabetes, such as neuropathy, nephropathy, and retinopathy.
High insulin prices can also strain the healthcare system by increasing costs associated with medication non-adherence, including hospitalizations for diabetes-related complications. Insulin price reductions and biosimilars may help alleviate this burden and make healthcare systems more sustainable in the long term.
PFLIEGER: Capping the cost of insulin has a significant impact on affordability, particularly for those patients on high deductible plans, which should have a positive impact on patient adherence. The sudden drop in insulin prices did not come without some casualties, as some pharmacies and suppliers absorbed the impact of the drop in value of on-hand inventory. To create positive, viable change it is important to look at impact on all players fairly including consumer, pharmacies, distributers, buying groups, PBMs, payors and manufacturers. Our healthcare system is highly complex, and in order for future innovation to be possible we must have sustainable business.
DESAI: Ensuring medications are affordable is critical to helping ensure medication adherence and chronic disease management. Insulin price reductions and new biosimilars can help some patients with the cost of their medications which we believe can remove a barrier to care and can result in better outcomes for those managing chronic diseases.
How much are smart insulin pens helping?
LYONS: Smart insulin pens have several benefits for patients with diabetes who are doing multiple daily injections. From a physical standpoint, they help patients avoid feeling tethered to their pump and integrated smart devices can titrate doses more exactly to get blood sugars into the range more quickly and keep them there. From a patient safety aspect, they allow more control without skill. The ability to connect to dose calculation apps and dose tracking capabilities help prevent insulin stacking mistakes, which is especially impactful for younger users.
DESAI: While uptake of smart insulin pens is still relatively low, we believe these products can be helpful to those who struggle to stay compliant with their therapy.
PFLIEGER: Smart or “connected” insulin pens offer a tremendous amount of promise, yet adoption has been slow. To a certain degree this is to be expected, it is never easy to launch a new technology into the US healthcare market.
Initial adoption is often slowed by insurance coverage gaps, and in the case of smart pens, healthcare professionals may be unsure of how to go about prescribing these devices since they require a specific pen or cartridge in addition to the smart pen and pen needles. While these devices make injecting a much easier, safer process the initial education, training and setup process can be intimidating and present hurdles too. As prescribers become more familiar with the platforms, and have positive experiences prescribing them across insurance plans these barriers will lift.
For those early adopter patients that are using smart pens, the device reviews seem positive. Endocrinologists that are familiar with the platforms also appear to value the connectivity they provide with the healthcare team, with studies showing that these devices can help overcome many of the challenges that come with multiple daily injections (MDIs) including dosing errors, prevention of “stacked doses” and reduction of hypoglycemic events.
The utilization of these devices is expected to grow significantly over the coming years, and when it does the benefits will be great. It’s going to take a little more time and patience. For new technologies to gain traction it takes can take years—from payor hurdles to product awareness, there’s just no quick way around it. Fortunately, coverage has improved and awareness is growing and these connected devices are finally starting to show some lift.
ZIVAN: Smart insulin pens are great options for people with diabetes who are taking multiple daily injections (MDI). These devices can support diabetes management via: dose tracking, dose accuracy, reminder and alert systems. integration with CGM, and remote monitoring and support.
In addition to the benefits of smart insulin pens, we see areas that need attention to ensure people with diabetes get the treatment they need, including:training/education on how to use the device, technological complexity, insurance coverage/cost barriers, and compatibility issues with smartphone and device.
Pharmacists can play a part in addressing these areas by engaging, educating, and equipping their patients with the knowledge they need to effectively manage their diabetes. It is important to remind patients to follow proper injection technique, including using a new pen needle for every insulin injection, and ensuring they have enough supplies to do so.
FREEDMAN: Smart insulin pens combine technology features like dose calculation and tracking, reminders, alerts, data integration and reports with the established accuracy, safety and convenience of insulin pens to help people with diabetes better manage insulin delivery. In addition, they create opportunities for healthcare providers to have a more complete picture of insulin dosing behaviors — allowing more informed, personalized data-driven treatment recommendations to improve diabetes management.
Despite their advantages and abilities to reduce some of the challenges of multiple daily insulin injections and improve patient outcomes by optimizing insulin delivery and reducing dosing errors, only a small percentage of insulin users are currently using smart insulin pen devices.
KERLEY: Smart pens can help users who require multiple daily injections to overcome the major challenges of dosage calculations and timing. They offer many features of an insulin pump, at a lower cost and without the inconvenience or discomfort of having a device attached to your body.
A smart insulin pen can calculate doses based on current blood glucose level, carbohydrate amounts, meal size, active insulin, and settings prescribed by a physician; deliver more accurate half-unit doses; help customers prevent skipped or missed doses; andConduct automatic dose calculation based on food intake or in response to a high blood glucose reading.
It can also track dosing and generate reminders for next doses; monitor insulin expiration and temperature ranges, so customers can replace the cartridge share data directly with the user’s health care team; and sync with smartphone or watch, and diabetes data tracking platforms.
KETTERLING: We have not seen a large growth of smart insulin pens in our geography, but do see how these devices could be valuable, allowing pharmacists to provide more real-time coaching, adjustments, and support to maximize therapeutic effects. As we continue development of remote therapy monitoring services, I believe we’ll see the prevalence of these increase.
HOUSTON: This all goes back to technology. When all of your information is connected across a smartphone, an insulin pen and a diabetes tracking platform, it helps improve adherence. The data helps patients manage insulin, food and physical activity and provides them with insights into how to best manage their insulin dosage as well as how they’re feeling.
Technology provides a huge benefit to patients — it helps them better manage a complex condition and leads to better outcomes. Rather than manually calculating information. The insulin smart pen does the math for you.
According to a study from IQVIA, patients with diabetes often report difficulty in managing their blood glucose levels and insulin dosing. The report found that insulin smart pens ease this burden on patients by automating many tasks associated with delivering insulin. The pens can also transmit insulin dosing data to a patient’s treatment team.
This all goes back to pharmacists being aware of the latest technology and resources for patients with diabetes and being able to provide education to help a patient navigate how to use a new device, such as a continuous glucose monitor. Pharmacists are truly a critical resource for communities and for patients managing complex diseases such as diabetes.