Last month, one furloughed government worker made national headlines by saying she had to ration her insulin because she couldn’t afford her co-pay, nor the ER bill, during the government shutdown. Recalling a day where her blood sugar was high, she admitted, “I just went to bed and hoped I’d wake up.”

Dave Chase
This is not how health care should work. And yet, Mallory Lorge is not the only American to have faced such a decision. According to an UpWell Health survey of 5,000 Americans with diabetes, 45% said there have been times where they couldn’t afford care and therefore went without it.
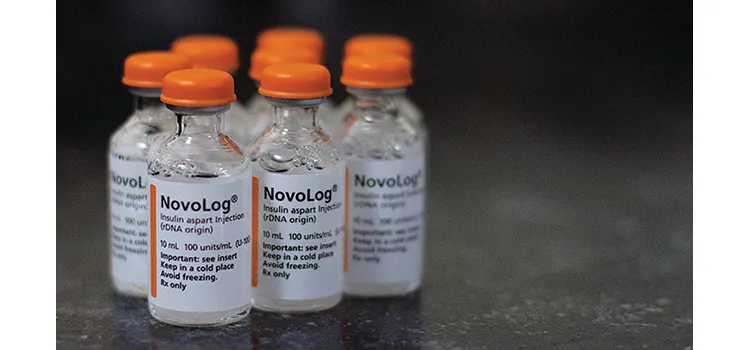
In protest of high prescription prices — in 2016, individual type 1 diabetes patients spent $5,705 on insulin — many people have pointed their finger at pharmacy benefit managers. PBMs act as middlemen between drug manufacturers and insurance carriers, negotiating rebates off of drugs’ list prices to reduce consumers’ costs at the pharmacy counter. Unfortunately, some PBMs have abused their power by pocketing those rebates instead of passing the savings along to consumers. Once they realized what was happening, lawmakers in West Virginia, Ohio, Pennsylvania and other states took matters into their own hands, and at the end of January the Trump administration issued a proposal that it hopes will increase market transparency and directly deliver discounts to consumers.
While pushing for a less opaque health care system is absolutely essential, there’s a misconception out there that all PBMs behave in this villainous way. No doubt there are some that deserve the association, but there are others that fulfil a positive purpose through transparent pharmacy benefits (TPB), a health plan component that employers can implement to reduce their spend and ensure employees have affordable access to the life-saving prescriptions they need.
One hundred fifty million Americans have employer-provided health insurance, and as such, what people pay for their prescriptions largely depends upon their employer’s health plan design. Given that people with diabetes on high-deductible health plans wait longer to get care than those on low-deductible plans according to a recent study from the Annals of Internal Medicine, it is critical that employers pay attention to their health plan’s inner workings.
Fortunately, most health plans already incorporate some sort of PBM, so rather than completely starting from scratch and having to design a new one, a deceptively simple workaround is all that’s needed to provide better pharmacy benefits at a fraction of the cost. The problem is — as news sources have exposed in recent months — that many of these PBMs aren’t actually working in the best interests of employers and their employees, even though it may appear that that is the case.
For example, in PBM-purchaser contracts, PBMs list drugs’ alleged average wholesale price (AWP): what retailers pay, on average, to buy a drug from a wholesaler. PBMs then say that they are able to secure a certain percent discount off of that price, making it seem as though they’re helping consumers save tens, hundreds, even thousands of dollars on their prescriptions.

However, AWPs can result in per-unit cost variability and open the door to even more manipulation — as per-unit prices go up, PBMs may claim it’s just part of the employer’s “cost trend,” when PBMs are actually raising prices to increase their own revenue. In such situations, it’s too difficult for health care purchasers to see what they are actually spending their money on and whether they are being priced fairly. Fortunately, PBMs are held more accountable in a TPB model because employers have access to their own data. This will prompt them to question anything that might seem suspicious, and in turn make pharmacy benefits decisions that best suit their employees’ needs.
For people like Mallory Lorge, prescriptions aren’t optional — they’re a matter of life or death. No American should have to pause before filling a life-saving prescription simply because they can’t afford it. Contrary to popular belief, PBMs can actually help in a TPB model, though to do this they must clearly negotiate costs and truly act in people’s best interests.
Dave Chase is cofounder of Health Rosetta, which aims to accelerate the adoption of simple, practical, nonpartisan fixes to our health care system. He is also the author of The Opioid Crisis Wake-Up Call: Health Care Is Stealing the American Dream. Here’s How We Take It Back.