ROCKVILLE, Md. — Last year, retail pharmacies greatly accelerated implementation of technology for electronic prescribing of controlled substances (EPCS).
Eighty-two percent of U.S. retail pharmacies are now EPCS-enabled, up 21% from 2014, according to a report released Thursday by e-prescribing solution provider DrFirst. Nearly all states have at least 60% of retail pharmacies EPCS-enabled, with over half of states having more than 80% of retail pharmacies capable of accepting and processing EPCS orders.
“This rapid expansion is driven in part by the increase in EPCS enablement by large national chains, such as CVS, Walgreens and supermarket-based pharmacies. It’s also due to increased recognition among pharmacy executives that EPCS is now legal in their resespective states,” DrFirst stated in the report, titled “The Evolving EPCS Landscape 2016: A Prescription for Stopping Opioid Abuse.”
Massachusetts, Michigan, Oklahoma, Rhode Island and New York currently have 90% or more of their retail pharmacies EPCS-capable. Some states that lagged in EPCS adoption in 2014 have improved significantly over the past 12 months, DrFirst reported. They include North Dakota, which rose from 22 of pharmacies enabled in 2014 to 73% last year, and Montana, which improved from almost zero enabled pharmacies in 2014 to 68% in 2015.
EPCS eliminates the risk of forged or altered paper prescriptions and sets up protections against fraud, doctor shopping, overprescribing and improper dispensing of medications due to misinterpreted handwriting. In its study, DrFirst noted that Massachusetts (90% pharmacy-enabled for EPCS) was the first state to implement EPCS. That came via a collaboration of the Agency for Healthcare Research and Quality (AHRQ), the state’s Department of Public Health, Brandeis University, Emdeon and DrFirst, which together conducted a three-year EPCS pilot in western Massachusetts that led to EPCS being legalized federally in 2010.
New York has the highest EPCS enablement in the nation, at 96% of the state’s retail pharmacies. This Sunday, New York will become the first state to legally require that all medications be prescribed electronically when its Internet System for Tracking Over-Prescribing Act (I-STOP) goes into effect.
Source: DrFirst Rcopia e-prescribing system pharmacy data, 2014-15.
Aimed at reducing rates of prescription drug abuse, the law requires medical providers to query the state prescription monitoring system (PMP) and review a patient’s recent medication history before writing a Schedule II-V drug prescription. That phase went into effect in 2013. In addition, I-STOP mandates that all prescriptions — noncontrolled (or legend) drugs and Schedule II-V controlled substances — be sent electronically as of March 27.
“However, EPCS is not widely adopted by doctors. On average, just 5.8% of all U.S. practitioners are currently EPCS-enabled,” DrFirst said in its report. “Even in New York on the eve of its I-STOP mandate, only 27% of practitioners are EPCS-enabled to date.”
According to the O ffice of the National Coordinator for Health Information Technology, at least 70% of physicians now send most prescriptions electronically, DrFirst reported in its study, highlighting the disparity between e-prescribing of noncontrolled drugs versus controlled substances. Many doctors aren’t aware that they can now prescribe all medications electronically, while others are reluctant to use the new technology or think it will be too expensive and time-consuming to deploy, DrFirst said.
“The slow rate of provider adoption of EPCS is surprising, given the compelling patient safety benefits and convenience of EPCS,” DrFirst chief strategy o fficer Tom Sullivan, a cardiologist, said in the report. “I expected that once EPCS was made legal in all states and EPCS-enabled pharmacies became prevalent, providers would quickly adopt this important tool. Clearly, more education is needed about the significant benefits of EPCS.”
One way to spur health provider adoption of EPCS technology is increased drug information exchange among state prescription drug monitoring programs (PDMPs), now operating in 49 states (except Missouri), DrFirst’s study said. Twenty-two states with PDMPs require providers to access the system before prescribing painkillers, though state laws vary widely, the report noted.
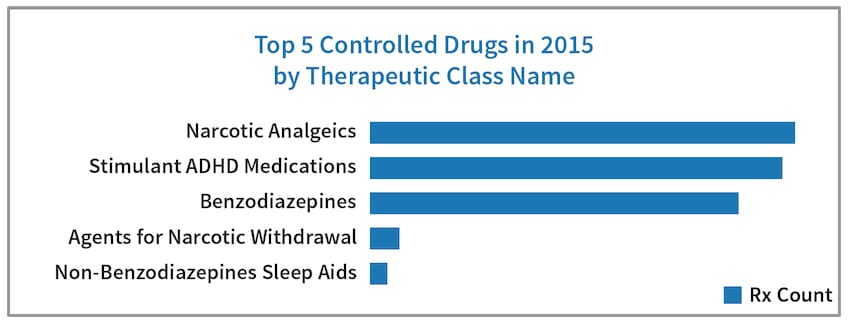
“Prescription drug monitoring programs create an environment of accountability for prescribers and dispensers,” Nick Barger, principal pharmacist at DrFirst, commented in the report. “Many controlled substances are uniformly recognized as high-risk medications. PDMPs provide an opportunity for prescribers and dispensers to collaborate on management of patients taking these high-risk medications.”
The DrFirst report said that a year aft er New York began requiring providers to check its online registry, the number of opioid prescriptions fell 10%, with the biggest declines for hydrocodone (down 20%) and codeine (down 33%).
“Twenty years ago, most people who were diverting or abusing drugs were getting their prescriptions illegally from stolen or forged and altered paper prescriptions. Today, most of the diversion and drug abuse comes from licensed physicians writing legitimate prescriptions for patients with acute and chronic pain problems,” Sullivan explained in the study. “Pharmaceutical companies have manufactured more and more powerful opioid analgesics that are easy to administer, inexpensive and with a plentiful supply. Patients can easily become addicted if not properly monitored.”
Drug overdoses are now the top cause of death from injury in the United States, with about 44,000 overdose deaths each year, DrFirst noted, citing data from the Centers for Disease Control and Prevention. The CDC has declared prescription painkiller abuse a national crisis, with 44 people dying from a prescription painkiller overdose daily. From 1990 to 2010, opioid overdose deaths more than tripled, and the number of prescription painkillers prescribed and sold in the U.S. has nearly quadrupled since 1999.