Insulin price cuts have raised awareness of the manageability of diabetes with monitoring and treatment. But given the stubborn increases in the disease’s prevalence and its worrisome side effects, education is still a must, which is where pharmacists can play a vital role. In this virtual roundtable, retailers and suppliers discuss how pharmacists and the latest technologies and products can help stem nationwide increases in diabetes and prediabetes.
To what extent have the price cuts by major insulin manufacturers, and the availability of Lantus biosimilars, raised public awareness of the ability to control diabetes cost effectively?
KETTERLING: Insulin price cuts and the approval insulin biosimilars have lead to increased patient access to insulin therapy and decreased the frequency of patients rationing their supply, and have allowed for appropriate prescribing habits and escalation of therapy if indicated for patients. Public awareness of the more affordable options amongst patients, providers and pharmacists helps mitigate cost as a barrier to appropriate diabetic therapy and, in turn, we should anticipate more diabetic patients making progress towards meeting their goals of therapy.

Kevin Duvall, Associate Director, Strategic Customer Marketing, embecta
KERLEY: Since the Inflation Reduction Act set a cap on the cost of insulin prescriptions per month for Medicare beneficiaries, there has been continued pressure from the public and government to lower prices for more persons with diabetes.
DUVALL: Type 2 diabetes is a progressive disease that may eventually lead to insulin therapy; most people who are diagnosed begin their treatment with other interventions, like diet and exercise. But the previously high cost of insulin was definitely the focus of a lot of attention and some backlash. Those high costs, combined with the costs of additional medications and supplies used by patients with diabetes, may have kept some people from fully utilizing the treatment. As the cost of insulin comes down, perhaps more prescribers and patients will utilize insulin as a treatment option sooner rather than later in the treatment pathway. One caveat to the increased insulin usage will be ensuring people with diabetes have access to education — particularly when it comes to proper injection technique 1and all it entails, including new needle usage — in order to gain the full benefits of the medication.

Phyllis Houston, Vice President, Pharmacy Enablement and Performance, AmerisourceBergen
HOUSTON: Overall, the price reductions on insulin from several major manufacturers have reduced the price burden on patients and given patients more control to effectively manage their diabetes.
Price reductions on insulin products have relieved financial pressures for patients who use insulin. Typically, there are many patients who have struggled with the high cost of insulin, who have not consistently followed best practices for insulin use, and due to the impact of reduced costs, they may not have to make those choices going forward.
Additionally, this price reduction has raised awareness that there are additional therapies and medications available to treat some types of diabetes.
ROOKER: Cost has really been the challenge for many patients trying to manage their diabetes effectively. This is a new biosimilar, and it will take time to create more market awareness and penetration. Helping patients reduce and control some cost in an expensive condition will only help with their treatment consistency.
LYONS: Cost is always a factor for patients when managing chronic conditions, especially in uninsured/underinsured individuals and those with high-deductible insurance plans. Anytime positive information about lowering costs for medications makes the news, it will spur conversations between patients and all health care providers, especially pharmacists. We are definitely seeing more conversations.
Actions taken to lower the cost of certain insulin products are a step in the right direction to help more patients achieve better outcomes and quality of life through greater adherence. As each patient’s treatment plan is unique based on a number of factors, my hope is this will inspire cost reductions for all diabetes medications, supplies, and up-to-date monitoring technologies.
CHO: We will see once the price cuts are enacted, but without doubt, the diabetes population will be better served through greater access.
How much is that translating into increased demand for diabetes patient education and support from pharmacists?
KERLEY: Pharmacists are one of the most accessible health care providers available to engage with customers regarding questions and/or concerns they may have about diabetes. Pharmacists and pharmacies are uniquely positioned to offer resources to help successfully achieve these lifestyle goals through services and product offerings at the pharmacy — including comprehensive medication reviews, identifying risks for developing diabetes or signs of prediabetes, and immunizations.
HOUSTON: The increasing prevalence of diabetes in the United States, coupled with recommendations from the American Diabetes Association that a team-based approach is the best way to manage diabetes will result in more patients demanding access to health care providers who can provide meaningful care and self-management tools.
The pandemic placed a spotlight on the impact pharmacies and pharmacists have on health outcomes. They are an underutilized but growing and accessible health resource in the community. Pharmacists are also on the front lines with patients daily, sometimes even seeing patients more frequently than their own health care provider sees them. This gives pharmacists the ability to recognize gaps in care very quickly.
We’re seeing that patients want to take ownership of their health care and mitigate cost barriers, and pharmacists are playing a central role in helping patients in this regard. Pharmacists can look at adherence issues, educate the patient on diabetic care, conduct preventive screening and provide information on how and when to test blood sugar.
Pharmacists can also advise on the impact of diet and exercise on diabetes and share the latest information on diabetes preventative care, the importance of kidney and eye exams, and the latest therapies and control measures.
This high touchpoint between pharmacist and patient allows for pharmacists to recognize more quickly when there is a gap in care, resulting in improving care and reducing overall health care costs.

Kelsey Rooker, Senior Advisor, Clinical Services, Outcomes
ROOKER: Diabetes is constantly evolving. There have been constant changes to monitoring, new product development, apps, food management and wearables for tighter monitoring and control. There is a lot of information being provided to consumers.
We are hearing how providers (prescribers, pharmacists and others) and patients alike are in need of more education about these examples, especially biosimilars, and the regulations surrounding them. Consumers see their pharmacists frequently and they are accessible, as nine out of 10 people live within five miles of a pharmacy. This correlates with being a trusted provider by consumers that can and are willing to deliver important content to better manage this condition.
DUVALL: Retail pharmacists are in a unique position to provide education as they usually see a patient several more times per year than other health care providers. Pharmacists have access to when patients are filling new/refilling medications and can counsel and educate these patients. To provide this education, pharmacists need to be armed with the appropriate information. Retail pharmacists have the opportunity to become the diabetes education hub, meaning either providing the appropriate education to the patient or directing the patient to the appropriate HCP and/or resource.

Nancy Lyons, Chief Pharmacy Officer, Health Mart
LYONS: Diabetes education and self-management training are critical parts of care for every patient living with diabetes and prediabetes. All health care providers know the value of getting patients enrolled in education, prevention and support programs early. The need is clear, especially with the therapy changes that may result from the cost lowering of some insulins. The demand, however, is also linked to costs for the patient. The available supply of high-quality, convenient and accessible diabetes prevention education services programs that are covered as a part of the patient’s benefit is limited.
Removing coverage barriers for patients to receive convenient and high-quality diabetes education from pharmacists is a logical and cost-effective next step to improve the health of patients living with diabetes. For example:
- Pharmacy locations are centrally located in communities with 90% of all Americans living within five miles of a community pharmacy, which often offer extended and weekend hours.
- Patients visit community pharmacies much more frequently than primary care offices.
- Pharmacists are well prepared to provide structured diabetes education, training and prevention programs and manage the ongoing emotional, behavioral and motivational aspects of living with chronic conditions.
- Pharmacists can also directly monitor and impact medication adherence and collaborate with the rest of the patient’s health care team to address barriers, solve problems and improve outcomes.
To be sure this can happen, pharmacists must be able to easily access adequate payment for diabetes care, education and prevention services. Barriers to billing need to be removed to ensure pharmacies can offer sustainable services.
During the COVID-19 pandemic, people living with uncontrolled chronic conditions including diabetes, experienced poorer outcomes, including higher rates of death. The health care industry has a responsibility to learn from the occurrences of the past and make changes to the way care and education are provided in the future.
LEBLANC: Patients have more access to information now than ever before. However, pharmacists are essential to helping patients navigate this information and, more importantly, to helping them understand how it relates to their diabetes management journey. Pharmacists are the main health care provider communicating with the patient when they switch to a biosimilar, and so are best positioned to provide diabetes support to patients. The switch is a perfect opportunity for pharmacists and patients to have a dialogue about diabetes management, complete a medication review if appropriate, and schedule follow-up education sessions with the patient as needed.
Pharmacists are an important part of a patient’s overall health care team, and with their accessibility, have one of the biggest opportunities to interact and help these patients in community setting. Our pharmacists have been leveraging tools available to them, like diabetic medication reviews, point of care testing for A1c and lipids and educational follow-up discussions to provide more proactive and preventative care to patients with chronic diseases including diabetes. Access and funding are some of the barriers patients with diabetes face, and our pharmacists have an incredible opportunity to help remove some of these barriers so patients with diabetes can better manage their condition.

Samantha Ketterling, Manager of Clinical Pharmacy, Thrifty White Pharmacy
KETTERLING: The approval of biosimilars alone has required additional education and support for pharmacists to evaluate for appropriate interchangeability and/or assist with the selection of cost-saving alternatives to patients.
We can anticipate that with lower-cost insulin solutions, more patients may be prescribed insulin. Insulin therapy requires pharmacist education on regular blood sugar monitoring, correct administration technique, safety monitoring, lifestyle coaching and diabetic preventative health care screenings. In turn, this has translated to increased demand for thorough drug utilization reviews, diabetic education, regular medication counseling and ongoing therapy monitoring by pharmacists.
How are retailers and suppliers collaborating to optimize pharmacists’ work with diabetes patients?
EMMONS: Diabetes is a complex health issue, and patients can be overwhelmed with its demands. Walgreens is committed to helping the diabetes community start and maintain an optimal regimen and routine to live a healthy life as a trusted member of their health care team, offering enhanced services focused on expanding access to affordable, local care. We invest in special training to equip pharmacists with expert knowledge about medications, continuous glucose monitors (CGMs), nutrition, how to keep A1c and blood glucose levels on target, and more. More than 20,000 pharmacists have completed this training to date.
LEBLANC: With aligned objectives to provide better and more proactive care for patients with diabetes, we believe pharmacists and their accessibility can help improve patient care and outcomes as access to primary care continues to be challenged. Working together with suppliers where it makes sense will allow us to combine our strengths, increase our reach, and improve patient experience and health outcomes.
DUVALL: As a former retail pharmacist, I felt I always needed to know “a little about a lot” when it came to medications and disease states. To gain the most up-to-date information on specific topics I partly relied on manufacturers. Retailers and suppliers have the opportunity to collaborate to provide, as the end goal, the best outcomes for the patient. To achieve that goal, suppliers can provide educational tools and resources not only for patient usage but also for information to educate the pharmacy staff on specific topics.
KETTERLING: Pharmacies and suppliers have collaborated on varying diabetes and education programs to support pharmacist’s accessibility and patient’s trust, including diabetes support programs, new start education, adherence monitoring and therapy optimization.
Additionally, there have been increased education and resources from insulin manufactures on approved biosimilars and cost-saving alternatives for pharmacies to utilize in their practice.
KERLEY: Medication adherence is important in reducing health care costs, hospitalization and mortality in persons with diabetes. Retailers and suppliers can collaborate on ways to drive adherence through personalized customer outreach.
ROOKER: Outcomes works with both retailers and suppliers, so we are positioned in the middle of this collaboration. Suppliers are partnering with retailers, often through vendors like Outcomes, to reach the patient and provider via different methods. We must engage both providers and patients where they are by leveraging multiple communications channels. This ensures we’re reaching them through their preferred channel and a method that works best for them. Pharmacists are receiving education via various channels, including information embedded within their clinical platform and other marketing programs. For example, the OutcomesOne platform delivers in-platform messaging around new products, workflow update and general enhancements to strengthen our network to help manage their patients. Patients also receive education through various channels, such as sponsored text programs and face-to-face educational conversations with their pharmacists; educational apps; and visits with their prescriber.
HOUSTON: Retailers and suppliers are collaborating to optimize pharmacists’ work in two ways.
First, education on the latest diabetes products allows pharmacists to effectively communicate with patients if a change may be needed for their care, and they can then collaborate with their provider on that prescribed therapy. There is a great understanding that this is an ever-changing marketplace with new solutions coming to the patients, so retailers and suppliers are continuously working to ensure that pharmacists are at the front edge of understanding the therapies available.
Second, retailers and suppliers are working on solutions and technologies that help identify adherence issues and that reach patients with adherence barriers. This includes mobile apps that make it easier for a patient to track A1cs, a common measure to track blood sugar control over time, for example. More generally, technology helps pharmacists more efficiently reach patients with important information like refill reminders.
There is also a large impact here on localized care — especially with the more than 2,300 independent community pharmacies that are part of AmerisourceBergen’s Good Neighbor Pharmacy network. There are opportunities for pharmacists at local independent pharmacies to build on their already close relationships with their patients to maximize care. Across the Good Neighbor Pharmacy membership, pharmacists know patients’ family members and have very strong community ties, and pharmacy staff often greet patients by their first name when they walk through the door. This results in the pharmacist being able to provide a higher level of care to patients they serve.
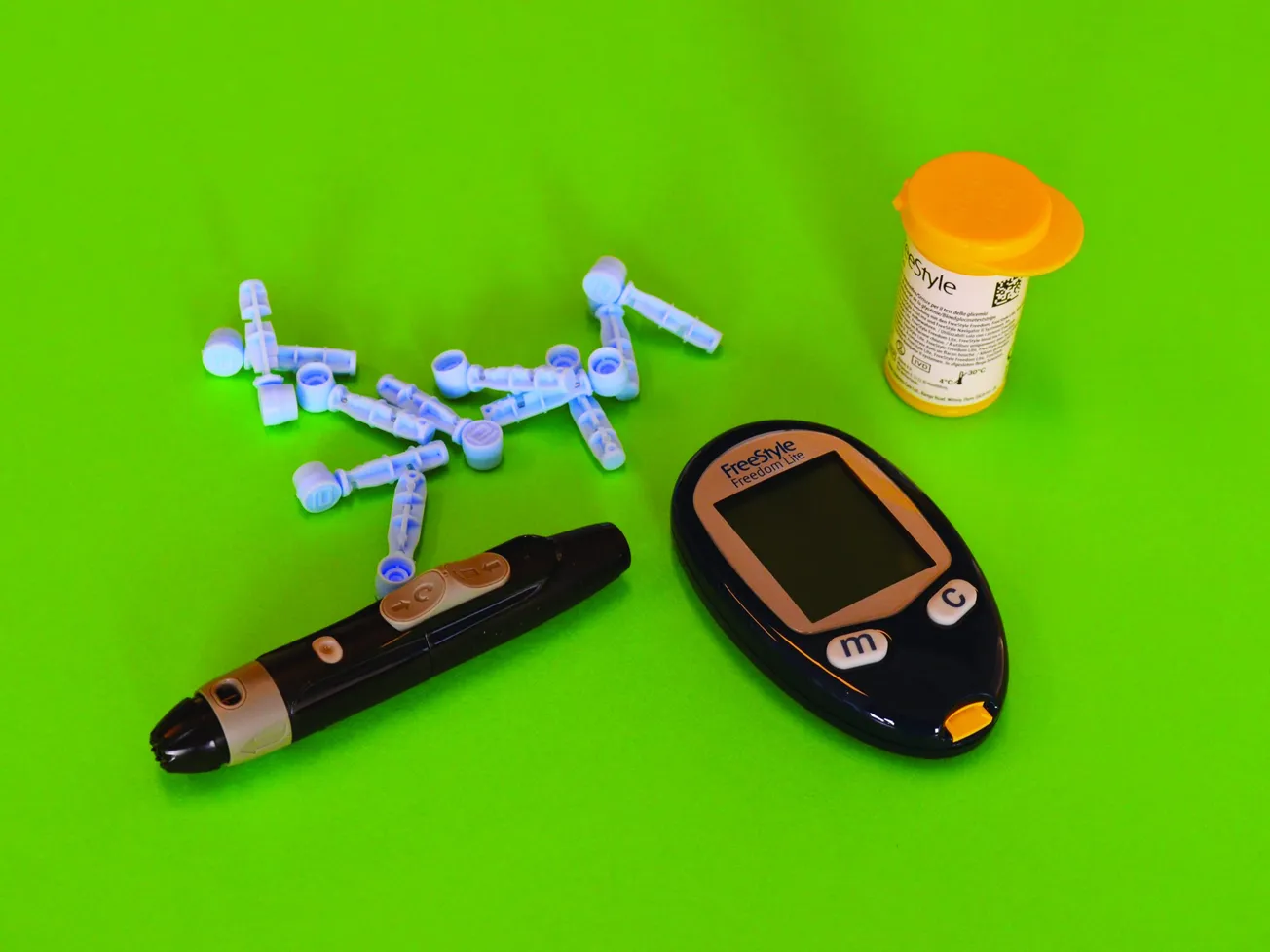
What new diabetes technologies/products hold the greatest promise?

Jake Cho, General Manager, AgaMatrix/i-SENS
CHO: The CGM has changed the game for people with diabetes. It is a far superior technology to the fingerstick process. The apps that accompany the CGM devices give remarkable insights to the patient and the physician. The expansion of CGM based bio-wearables into the wellness space will create a significant opportunity for pharmacies to create a metabolic health category that serves the health interests of the general population.
HOUSTON: CGMs and integrated glucose monitors are a really nice way for patients to ensure they’re consistently monitoring their glucose levels without having to frequently perform burdensome fingerstick blood checks.
This level of consistency and convenience is important for patients who are managing a very complex disease like diabetes.
These monitors allow patients to track blood sugar over a period of time so they can compare trends, analyze the impact of food intake and more quickly see the impact of those decisions compared with physical activity and taking their medication.
Additionally, the ability to connect these glucose monitors to smartphones and apps allows patients to have a more holistic approach to managing their total health outcomes versus managing diabetes by itself. It really allows that connection point across their entire life.
ROOKER: There is a lot of activity in the CGM space around policy changes towards access, new integrations and information pertaining the artificial pancreas. Managing diabetes through new AI methods is also a topic coming to the surface, and I really see this being a huge focus in the industry for the near future.
There is also a lot of buzz in the GLP-1 agonist and SLGT-2 inhibitor space that I foresee continuing, as well. I am looking forward to all of these products, because diabetes impacts over 37 million people, our population is aging, the type 2 population represents 90% to 95%, and these technologies and products will help the entire care team along with patients themselves predict and manage control.
LYONS: Alternative, connected patient monitoring devices that allow patients less-invasive methods of monitoring their blood sugar are very exciting. The changes in the clinical guidelines and the coverage for CGMs will open the door to better, more proactive control and reduced complications in multiple patients. The more sophisticated connectivity of multiple devices, including glucose meters, CGMs, insulin pumps, blood pressure devices, weight scales, and activity tracking and nutrition assessment applications, holds a lot of promise for better control of diabetes, as well. Many of the new technologies allow real-time data to be shared with pharmacists and other members of the patient’s health care team to facilitate team collaboration and coordination in the care of people with diabetes.
For example, connected glucose monitoring devices, blood pressure monitors, CGMs and insulin delivery devices can allow pharmacists to review trends and make better recommendations for medication adjustments. Registered dietitians can use the data to personalize nutritional plans, and physicians and other prescribers can review the recommendations and adjustments to ensure that all treatment goals are optimized, giving the patient more control and a better quality of life.
KERLEY: With the variety of new technological innovations becoming available, these new devices hold promise for making diabetes easier to manage. Advances such as continuous glucose monitoring are making the often-dreaded fingerpricks a thing of the past, while closed-loop systems help automate insulin delivery. Diabetes apps have emerged as valuable tools for people living with diabetes. It really comes down to the product that best meets the needs of the individual patient and helps make self-managing their health easier.
DUVALL: Numerous new diabetes technologies and products have come to market over the past two decades, including insulin pumps, CGM and injection devices, new classes of medications, improved mechanism of action of certain medications, among others. All of these have a particular place in diabetes treatment and management. However, the greatest promise of controlling diabetes doesn’t hinge on one particular technology or product but on patient ownership. Patients must want to manage their diabetes to control it. New technologies and products can assist with the control and, more importantly, help change patient behavior. However, providing a patient with a new product in the hope of changing behavior and/or blood glucose control without their buy-in to manage their diabetes will usually only produce minimal results with only short-term or no change in long-term behavior or control. As such, it is a combination of finding the right technologies and tools for the specific behavior to help patients change their behavior and management of diabetes.

Stacey Emmons,Director of Pharmacy and Retail Operations, Walgreens
EMMONS: Walgreens offers comprehensive expertise, services and products to support people living with diabetes:
- Expansive diabetes product offerings including a large assortment of Walgreens brand health and wellness items like blood glucose meters and testing strips, blood pressure monitors, vitamins and supplements, foot care products, and newly launched Walgreens brand pen needles that offer cost savings and fit all insulin pens on the market today.
- Largest provider of CGMs including the Dexcom G6 and FreeStyle Libre 2, which track glucose levels all day and night — fewer fingersticks required. These state-of-the-art health monitoring devices provide patients with real-time glucose data.
- Affordable care options and tools including Walgreens Prescription Savings Club and Find Rx Coverage, which offer insulin savings programs and affordable, predictable co-payments on select insulins. Walgreens Find Care provides access to in-person and virtual health care expertise from the comfort of one’s home.
LEBLANC: There are a lot of advancements in new pharma products as well as medical devices to improve patient experience and health outcomes. Some of the key promising areas on the technology side are:
- Real-time CGM systems — Empowering individuals with diabetes to make more-informed decisions about their insulin dosing and lifestyle choices.
- Insulin pumps — Advancements in insulin pump technology, such as automated insulin delivery and integration with CGM systems, have the potential to improve glucose control, simplify insulin administration, and provide more flexibility and convenience to users.
- Artificial pancreas systems (closed-loop systems) — Combining CGM and insulin pump technology with sophisticated algorithms to enable automated insulin delivery and dose adjustments based on real-time data.
- Mobile apps and digital solutions — Apps that are integrated with CGM devices and insulin pumps, and other diabetes devices to provide users with personalized insights, reminders and educational resources.
KETTERLING: Prescribing of CGMs and patient receptiveness to this nontraditional glucose monitoring have increased significantly. The value of real-time monitoring and accurate reporting to influence therapy optimization has been better realized by prescribers, pharmacists and patients. Further development of remote patient monitoring services and program implementation, specifically in pharmacies, holds great opportunity for pharmacists to play an integrate role on the patient’s health care team for chronic diabetes management.
Expanded health care technology, interoperability and streamlined referral process between pharmacies and primary care providers/health systems/health care resources will continue to bridge the gap between care providers and allow for diabetes care optimization and improvement in clinical outcomes.
Lastly, the use of GLP-1 receptor agonists has evolved significantly in the last year. This class of diabetes drugs is in high demand. GLP-1 receptor agonists are highly effective, which has led to recent clinical guideline updates to support the usage of this class. The American Diabetes Association now recommends injectable GLP-1 receptor agonists as first-line injectable therapy and the oral GLP-1, Rybelsus, as a first-line treatment for type 2 diabetes. New indications for use, cardiovascular risk reduction, social media trends, off-label usage and a change in prescribing habits have all lead to the increased demand of GLP-1s. The combination of these variables has led to varying drug shortages and temporary delay in initiation of therapy for some patients. However, once these variables balance out more evenly we will likely see the usage of this drug class continue to increase for the treatment of type 2 diabetes. Similar to the increased demand for diabetes patient education and support from pharmacists for insulin therapy, there will be an increased need for pharmacists to support the rise in GLP-1 usage, including additional administration education, side effect monitoring and lifestyle management (diet and exercise).
Why does the prevalence of prediabetes/diabetes continue to rise, and what part can pharmacies play in stemming the tide?
ROOKER: Education, education, education. Proactive communication and continuous support before, during and even post diagnosis. We must ensure patients are educated on how to live a healthy lifestyle, and when that isn’t enough, we have to lean on pharmacies and providers to help patients understand treatment options and the importance of adherence and assistance. Then, helping the patient determine which treatment option is best for their personal lifestyle is key, along with regular follow up on the efficacy of the selected treatment.
LEBLANC: There are a few key contributors to the increasing prevalence of prediabetes and diabetes. The first is the aging population in Canada and the increase in prevalence of chronic diseases like diabetes in the older population. Second, the pandemic has contributed to an increase in sedentary lifestyles and, unfortunately, an increase of unhealthy habits for Canadians, causing higher prevalence of obesity in Canada, which is one of the leading factors contributing to prediabetes/diabetes. Third, the increase of immigration in Canada will be a contributing factor to increased prevalence of diabetes as our Canadian population continues to diversify and certain ethnicities have a higher prevalence of diabetes based on genetic composition.
Over 5 million Canadians have prediabetes or undiagnosed type 2 diabetes. Early diagnosis and interventions can help reduce the overall progression of the disease. Pharmacists can help identify at-risk patients by playing a larger role in screening. Pharmacists are the most easily accessible health care providers and are uniquely positioned to screen patients in larger numbers and more frequently. Due to the growing prevalence of diabetes and increase in challenges with access to health care (one in five Canadians have no primary care provider, or are unattached, and that number is expected to continue to grow) pharmacists are an accessible health care provider that can help identify and help manage these conditions in the community with over 11,000 pharmacies across Canada.

Summer Kerley, Vice President, Clinical and Market Access Solutions, Rite Aid
KERLEY: There are many reasons contributing to the increased prevalence of prediabetes/diabetes. Examples include obesity, physical inactivity, family history and aging population. Since they are among the most trusted and accessible health care providers, pharmacists are an essential resource when it comes to information and education — including information about diet and other factors that can have a significant impact on how our customers with diabetes manage their condition. Pharmacists can also help monitor adherence to medication.
Rite Aid’s Medicine Support Team enables Rite Aid to reach customers who may not frequently be visiting our pharmacies to fill their medications. This type of outreach allows Rite Aid to remain connected to these customers and support behaviors that lead to better disease management and healthier lifestyles. Additionally, Rite Aid Rewards members have 24/7 access to a health care professional via online chat and over the phone (800-RITE AID) Monday through Friday from 9 a.m. to 8 p.m. EST.
KETTERLING: Contributing factors may include lifestyle choices, such as diet, physical activity, substance use disorders, and comorbid conditions. Additionally, barriers to care including access and other social determinants of health (SDOH). Pharmacists can have an impact by having more involvement in proactive screening for prediabetes/diabetes and assessment and referral processes for SDOH factors impacting diabetes care.
CHO: It’s 100% lifestyle — a deep-rooted and complicated issue that goes way beyond the scope of pharmacies. That said, any encouragement or education on healthy nutritional choices will help patients. Information and caring guidance is critical here.
DUVALL: Prediabetes/type 2 diabetes is a behavior-associated disease many believe mainly stems from poor nutrition and insufficient physical activity but may also be hereditary to an extent. With pharmacies being highly accessible by most Americans, with some located directly inside grocery stores, there is an opportunity to look at the patient holistically, and not just via their medications. This approach would tie food purchases and activity into the overall treatment plan that includes medications, procedures and other choices.
LYONS: Pharmacies and pharmacists can play a major role in stemming the rise in prediabetes/diabetes through prevention education, modeling positive lifestyle changes in the local community, leveraging social media to make movement and healthy eating fun and easier. Most importantly, pharmacists and their teams can help identify and remove barriers to health equity that result in the onset of diabetes.
In fact, Health Mart, McKesson’s pharmacy network, is working to coordinate programs and solutions that will leverage all the expertise found at the community pharmacy to work at the top of all licenses and credentials. In May, Health Mart launched HealthMart.FindHelp.Com, a closed-loop SDOH referral system that will allow any member of the community to access information about local resources for transportation, child care, mental health, food and nutrition services, and more that can impact health outcomes. Health Mart pharmacies can leverage the tool to make and follow up on referrals with patients.
HOUSTON: There’s a lot that contributes to the prevalence of prediabetes/diabetes, including diet, exercise and access to healthy food choices. But what’s clear is the disproportionate burden of diabetes on communities of color. In fact, the prevalence of type 2 diabetes and the underlying risk factors can often be linked to SDOH, which are a complex web of conditions that determine a patient’s health risks and outcomes, including where people live, learn and work. For communities of color, there are several risk factors that can be barriers to both preventing the onset of diabetes and effective diabetes management, such as a lack of access to health care; limited access to healthy and nutritious food choices; and other lifestyle factors.
Additionally, when looking at patients living with diabetes, they frequently report financial stress related to the cost of insulin, food insecurity and housing instability. Due to the complex nature of diabetes, patients often need an accessible, culturally competent care team to build patient/provider trust to manage their overall disease state more effectively for better health outcomes.
According to the CDC’s 2020 National Diabetes Statistics Report, when compared to non-Hispanic whites (7.5%), rates of diabetes among diverse populations are as follows: American Indians/Alaska natives (14.7%), Hispanic Americans (12.5%), African Americans (11.7%) and Asian Americans (9.2%).
What’s more, American Indians and Alaskan Natives are routinely understudied in large-scale health data collection efforts, so it is more challenging to estimate the prevalence of undiagnosed diabetes in this population.
Given these statistics, the American College of Physicians and the American Diabetes Foundation are now recommending screening and addressing SDOH when caring for patients with diabetes.
Fortunately, pharmacists have already started to incorporate SDOH when caring for patients with type 2 diabetes. Pharmacists are looking to stem the tide of diabetes prevalence in communities of color by collaborating with local community organizations, churches and food pantries to promote healthier eating, exercise and diabetes management. They are also encouraging diverse patients to participate in diabetes research and are trying to understand the distinct differences in which different ethnic groups suffer from diabetes and how to better address and refine treatment for improved outcomes.
Discuss the possibilities for remission for type 2 diabetes and the role pharmacists can play in bringing it about.
KETTERLING: Beginning with integrated pharmacist involvement in diabetes care management, further development of patient collaboration of pharmacist-provided care can influence diabetic clinical outcomes results. Further development of pharmacist-focused efforts on controlling diabetes and helping achieve goals of therapy may help approach the possibility for remission of type 2 diabetes in the future.
KERLEY: Diabetes is a disease of progressive nature, so it is important to remember that once a person is diagnosed with type 2 diabetes, they always have the predisposition for the disease, which at this time is not considered reversible. With that said, Rite Aid pharmacists can be a part of the health care team that supports customers in reducing their A1c level to the level of someone without diabetes by educating them an array of topics such as self-monitoring, healthy diet, exercise, stress reduction and medication adherence.
Customers use Rite Aid’s Diabetes Solution Center as an additional resource for information and tools to manage their condition. We believe that education is the foundation of care, particularly when it comes to conditions like diabetes.
CHO: Early detection and a positive attitude are the two key factors here. If patients receive encouragement from any health care professional to take matters into their own control, then we can forecast improvement. Pharmacists can be most useful by having a local referral to nutritionists who can help guide the newly diagnosed towards lifestyle change. This is all very possible and requires a positive call to action.
HOUSTON: There are many ways pharmacists are working to manage disease states and help to identify where barriers exist that can lead to prediabetes and prevent remission of type 2 diabetes.
Some pharmacists are implementing community health workers, who are individuals within a pharmacy who become certified to help identify barriers and aid patients in overcoming them at a local level. Community health workers often come from the same neighborhood as patients and can connect with them more on a personal level than their doctors or other health care professionals would normally. These workers have also more information about local resources, such as church groups or transportation options where they’ll pick up patients and bring them to doctors’ appointments.
Additionally, through structured diabetes education programs, pharmacists can really enable and empower patients to better manage their disease. Pharmacists can also create a bridge with care plans to better connect patient, provider and pharmacist so there isn’t a gap in care ecosystems and there is a larger opportunity for pharmacists to intervene much more frequently and more quickly. This ability to share information between all parties that care for patients is still evolving, but it is an area that is continuing to grow with more pharmacists coming into the fold — as well as the recognition that pharmacists play a key role in the community as another health care provider.

Lori Leblanc, Vice President, Pharmacy Services and Strategic Initiatives, Shoppers Drug Mart
LEBLANC: While type 2 diabetes remission is possible in some cases, maintaining that over the long term requires significant changes in lifestyle. In most cases, the focus will be on preventative/proactive care that is possible to help manage the progression of the disease by identifying it sooner/earlier (i.e., prediabetes stages) and helping patients managing proactively to prevent the complications or delay as much as possible. Pharmacists can play a role in helping patients come up with an individualized plan for a healthy lifestyle that may involve weight loss and updates to their diet and exercise routine to manage their diabetes effectively.
LYONS: The opportunity to delay, prevent, and achieve remission for type 2 diabetes requires early and proactive lifestyle interventions and education. People with prediabetes can stop the progression to type 2 diabetes, and those living with type 2 diabetes can achieve remission by sustaining normal blood glucose levels for at least three months without taking diabetes medication. Research on why some patients achieve remission continues, but the most common explanations center around proactive response to glucose trends through active monitoring and modest weight loss.
Pharmacies can play a huge role in increasing proactive efforts to support lifestyle changes as well as management of chronic diseases like diabetes through the following activities:
- Offer education, awareness and screenings in central places of community gatherings such as schools, churches, barber shops, etc.
- Provide tailored education and individual self-care training sessions for glucose monitoring, blood pressure monitoring, injection technique and identification, prevention and treatment of hypoglycemia.
- Support lifestyle change education focused on smoking cessation, weight loss, physical activity and coping skills.
- Leverage resources available in the community, including public health officials and trained community health workers (CHWs) to assess and break down barriers and improve health equity. In fact, McKesson recently funded scholarships for 60 certified pharmacy technicians working in community pharmacies to complete a comprehensive 16-week CHW training program developed by CEImpact.
- Consider all SDOH factors that may contribute to the patient’s ability to care for themselves.
McKesson believes when community pharmacies engage in these diabetes prevention and treatment support activities, they can strengthen their business and elevate the role their pharmacy plays in people’s lives.
DUVALL: I’m not sure if type 2 diabetes will ever be eliminated from our society. However, I do think pharmacists can play a role in helping patients achieve not only blood glucose control, but also other health improvements. With the expanding roles and abilities of pharmacists to do more when it comes to educating, managing and even prescribing, they are in a unique position to make a huge impact in the overall health care landscape of the country. This critical impact can be achieved one patient at a time.
ROOKER: Pharmacists can best help guide patients toward remission through education and monitoring. Ensuring patients are educated and engaged in their diabetes treatment plan is critical — with pharmacists being one of the most accessible and trusted providers, they are well positioned for this task. Pharmacists are also well positioned to play a major role in helping patients adhere to their diabetes therapies. Pharmacists can recognize and identify patients facing these challenges, and whether through cost-reduction strategies, daily medication reminders, finding transportation, or offering delivery service, among other tactics, they can identify the best possible solution that addresses each patient’s individual challenges and barriers. Through Outcomes, pharmacists can also take advantage of messages and materials on retention and education provided by our manufacturer partners seeking to get these materials directly delivered to patients.