With growing disparities in health outcomes, health care leaders know that it’s important to continue working toward new solutions to improve health equity. But amid ongoing cost pressures and continued labor shortages, addressing health equity can get lost along the way. So, how do we ensure health equity remains a central priority for pharmacy retailers? This was the focus of discussion at the second annual Health Equity Summit, presented by Kearney and Chain Drug Review.

Laura Bowen
Who is affected by health inequity?
In the U.S., disparity in health care access and outcomes affects many marginalized populations. And the impact is staggering. People in the least affluent ZIP codes can expect to live more than 20 years less than their neighbors in the most affluent ZIP codes. Annual health care spend on white adult Americans is approximately 56% higher than for Black and Hispanic Americans. Black infants are two times more likely to die than white infants.
This inequity is heartbreaking, and it’s also expensive. It affects everyone, even those who aren’t in marginalized communities. The U.S. loses $42 billion in untapped productivity each year due to health inequities.
Equity + efficiency can work hand in hand
While leaders at most health care organizations will tell you their true purpose is to improve health for all, they feel relentless pressure to meet near-term financial goals — sometimes at the expense of health equity. Cost saving and efficiency become the focus of transformation efforts.

Dominique Harris
But what if improving health equity could also improve health care companies’ financial success? In fact, efficiency and equity can align powerfully as dual engines working together to deliver a healthier future for all. For example:
• Streamlined processes reduce administrative burdens, decrease patient wait times and free up resources.
The result: More tailored health care service delivery that meets the needs of underserved populations.
• Cost-effective prevention methods proactively manage health needs and facilitate early detection.
The result: Reduced long-term costs of care and improved outcomes for all.
• More efficient resource allocation allows organizations to invest strategically and distribute resources effectively.
The result: Health care services reach a broader population.
• Enhanced care coordination reduces redundancies and gets patients the care they need sooner.
The result: Better, earlier outcomes for all.
By making health equity the focus of transformation, health care companies will develop bolder visions, rethink their delivery models, achieve their mission of serving others, and establish profitable and scalable cost structures.
Equity requires a mindset shift

Rodey Wing
As we heard at the summit, organizations are already exploring a lot of great ideas and interventions to address equity. But knowing where to get started and getting stakeholder buy-in is challenging.
The first step is a mindset shift. Making decisions based on health equity requires a fundamental change in how everyone in an organization thinks. Improving health equity isn’t a side project; it should power every decision. Health equity-led transformations aren’t about being charitable, finding pockets of financial benefits or achieving short-term returns. They’re about fundamentally changing the business model, creating favorable business and health outcomes, and achieving long-term goals.
Consider these three important mindset shifts:
• From philanthropic effort to core business — Instead of considering health equity an act of charity, recognize the business benefits of focusing on health equity. Shift to prioritizing equity in every facet of business decision-making processes.
• From initiative-level gains to holistic portfolio improvements — Instead of reviewing the cost dynamics of individual initiatives, widen the aperture to account for business-wide benefits, future returns and improved outcomes.
• From immediate returns to long-term lower-cost structure — Instead of focusing on short-term cost savings, consider up-front investments that improve patients’ health and lower care costs in the long term, enabling structurally lower costs and a more sustainable and scalable operation.
Four key steps to get started

Karen Yocky
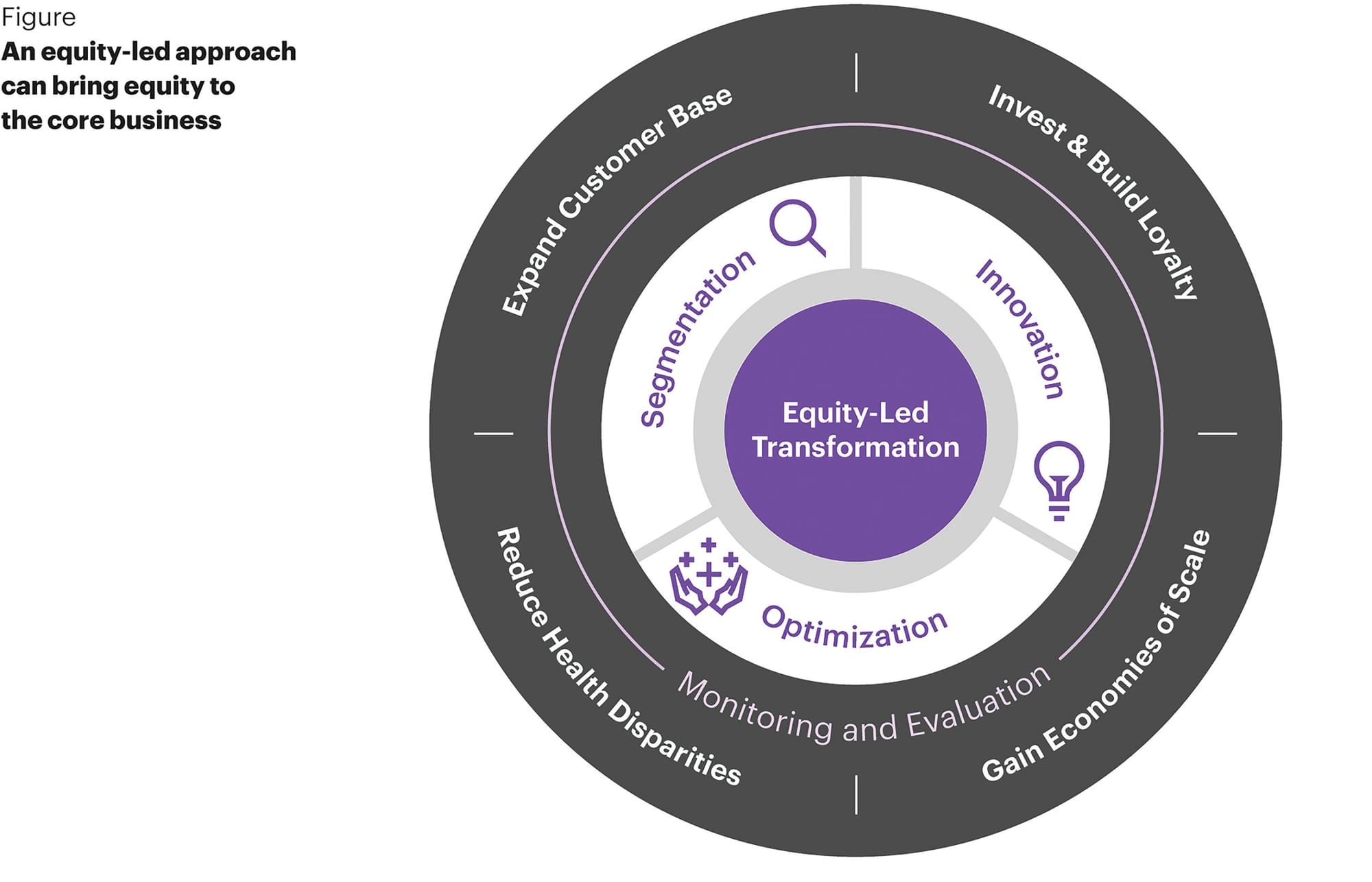
With those mindset shifts, organizations can then operationalize a more equity-led approach and bring equity into the core business. Discussion at the summit focused on breaking this into actionable steps to get started. (See Figure above.)
• Segmentation: Focus on populations with the highest need where you can have the biggest impact. You can’t be everything to everyone, so it’s important to focus on these critical populations.
• Innovation: We know the health care system isn’t meeting the needs of all patients. So how do we change or innovate the way we deliver care to ensure it meets the unique needs of these prioritized groups?
• Optimization: We’ll need to optimize the operating model and supporting structures to serve these segments sustainably and profitably.
• Monitoring and evaluation: Finally, it’s essential to monitor and evaluate the impact and value of these programs. The social return on investment (SROI) methodology is a helpful framework.
Centering equity in every facet of the business not only improves health outcomes but expands the customer base to new patients, builds deeper loyalty with patients and communities, and enables greater economies of scale.
At the summit, leaders reflected upon their energy and commitment to improving equity. The collective momentum made clear that when we collaborate across the health care value chain, shift our mindsets and take tangible steps in our organizations, we can create stronger organizations and communities for the long term.
Thanks to Beth Bovis, Todd Huseby and Katy Rauen for their contributions to this article.
Dominique Harris is a partner in the leadership, change and organization practice at Kearney, a global strategy and management consulting firm. She can be reached at dominique.harris@kearney.com. Rodey Wing is a partner in the health care and life sciences practice at Kearney. He can be reached at rodey.wing@kearney.com. Laura Bowen is a principal in the in the health care and life sciences practice at Kearney. She can be reached at laura.bowen@kearney.com. Karen Yocky is a manager in the in the health care and life sciences practice at Kearney. She can be reached at karen.yocky@kearney.com.









