By Karen Yocky and Rodey Wing

Karen Yocky
“You are what you eat.” We know that diet is a vital contributor to health. And now, new funding pathways from both the public and private sector are fueling even more momentum for Food is Medicine programs. In today’s shifting landscape of where consumers receive their health care, pharmacies can play a crucial role in the patient care journey. The pharmacy is becoming a destination for patients to test, diagnose, treat and manage health conditions. How can pharmacies play a central role in the growing Food is Medicine initiative?
New consumer research from Kearney shows that consumers are very open to food prescriptions, but as programs shift from pilots and discussions about funding, a more consumer-oriented design approach is needed. In this article, we’ll explore consumer perceptions of food prescriptions and outline actions to better position the pharmacy as a care provider in the food-fueled health movement.
Momentum is growing for Food is Medicine

Rodey Wing
In September 2022, the White House held the White House Conference on Hunger, Nutrition, and Health for the first time in 50 years and released a National Strategy on Hunger Nutrition and Health that put the integral connection between diet and health on a national stage. Since the conference, stakeholders across the public and private sectors have been mobilizing to activate these bold commitments to Food is Medicine. In February 2024, the White House announced its Challenge to End Hunger and Build Healthy Communities, with nearly $1.7 billion in new commitments toward nutrition and health, on top of more than $8 billion made alongside the White House Conference. Adding to that momentum, the Milken Institute and the National Association of Chain Drug Stores have partnered to uplift and support pharmacies in scaling interventions. These commitments underscore the urgency of addressing food insecurity and promoting well-being nationwide.
While traditional food-based interventions have ranged from more prescriptive (for example, defining a patient’s diet post-surgery) to more gentle (such as broad recommendations to eat healthier), the next era of food-fueled health will impact more and more patients, particularly for those using Medicare and Medicaid plans.
In particular, food prescription programs are one such intervention with the potential to have a large impact. A food prescription is a health program designed to improve health outcomes and access to food. Health care providers can screen, diagnose, identify and prescribe fresh fruits and vegetables to patients, completely free or subsidized to the patient and typically covered by health insurance. The prescription often takes the form of a voucher or coupon, which can be redeemed at participating local farmers’ markets, grocery stores or home delivery platforms.
How do consumers feel about food prescriptions?
The short answer: There’s a clear opportunity to educate patients about food prescriptions.
In November 2023, Kearney surveyed about 1,000 individuals across varying demographics and patient populations to better understand consumer perceptions of food prescriptions. Almost 75% of respondents were either entirely unaware of food prescriptions or did not know what they were prior to taking our survey. And while most believe that food prescriptions would be beneficial, there is some skepticism among healthier and older populations.
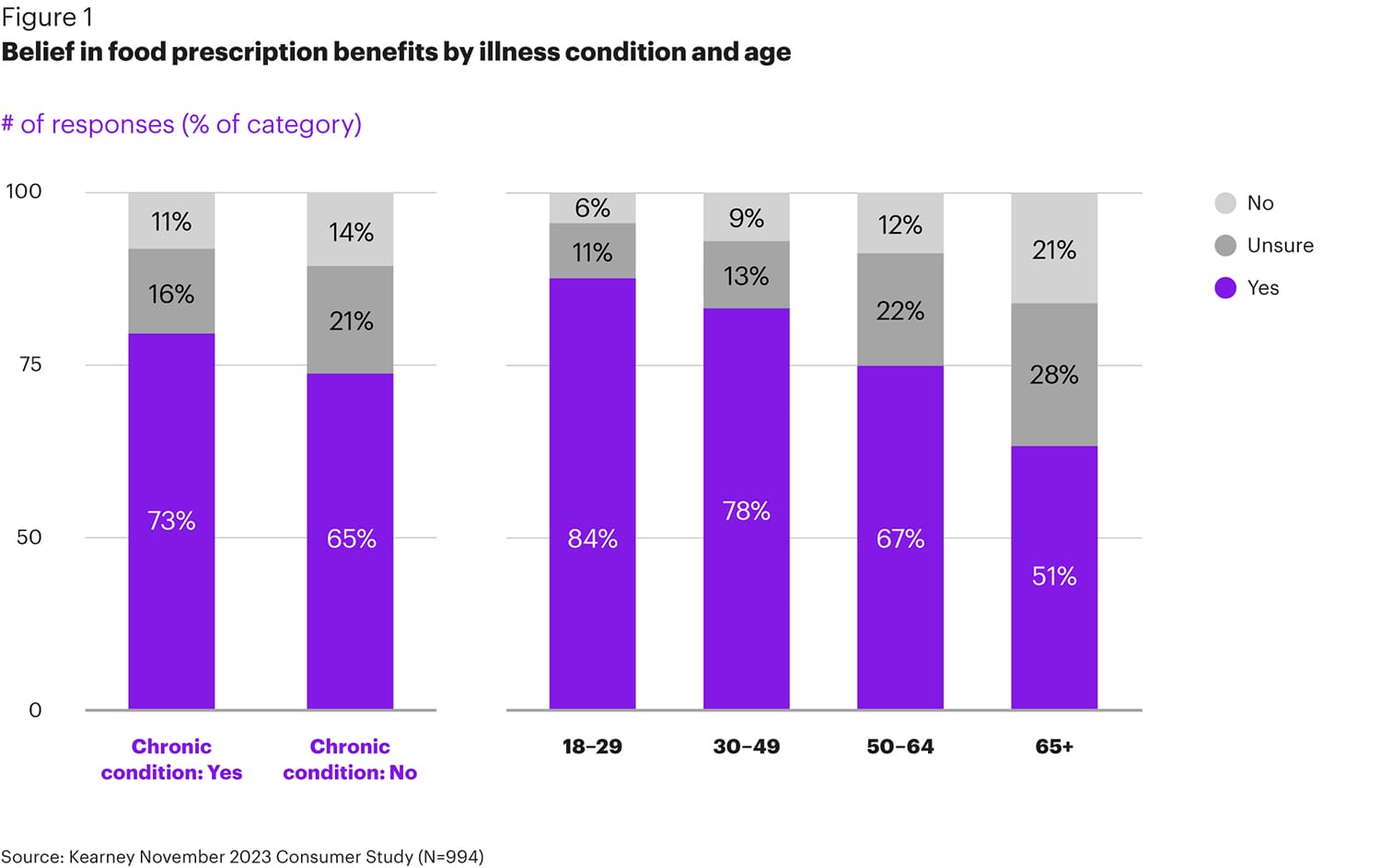
The groups that are most open to the benefits of food prescriptions are younger people and people with chronic conditions (see Figure 1). 73% of individuals with a chronic condition believe in the benefits of food prescriptions, falling to 65% for those without chronic conditions. 84% of individuals ages 18 to 29 believe in the benefits, dropping to 51% for those 65 and older.
One way to raise interest in food-fueled health is to rethink the naming and messaging. In our survey, “food prescriptions” weren’t as appealing to people as “healthy” food (see Figure 2). Consumers prefer program names that reference health and position the program as a benefit, not a direct order. People want to feel empowered to make healthier food choices, but they don’t want to feel like their health care team or government is controlling their food choices.
The program’s name may not seem important, but messaging will be a key tool to drive consumer perception, engagement and health outcomes. While policy makers and payers are comfortable with food “prescriptions,” consumers don’t engage with that word in the same way. So, as this model moves from a policy-focused campaign to a consumer-focused solution, there’s a clear need to evolve the language intentionally.
The takeaway for pharmacy leaders: As food prescriptions grow beyond the pilot phase, the messaging must evolve to resonate with a mass audience. For example, health care organizations should consider more education and outreach to boost participation, including targeting outreach by population groups to achieve broad awareness of food prescription programs and benefits and to build consumer confidence.
Food-fueled health offers convenience, variety and value
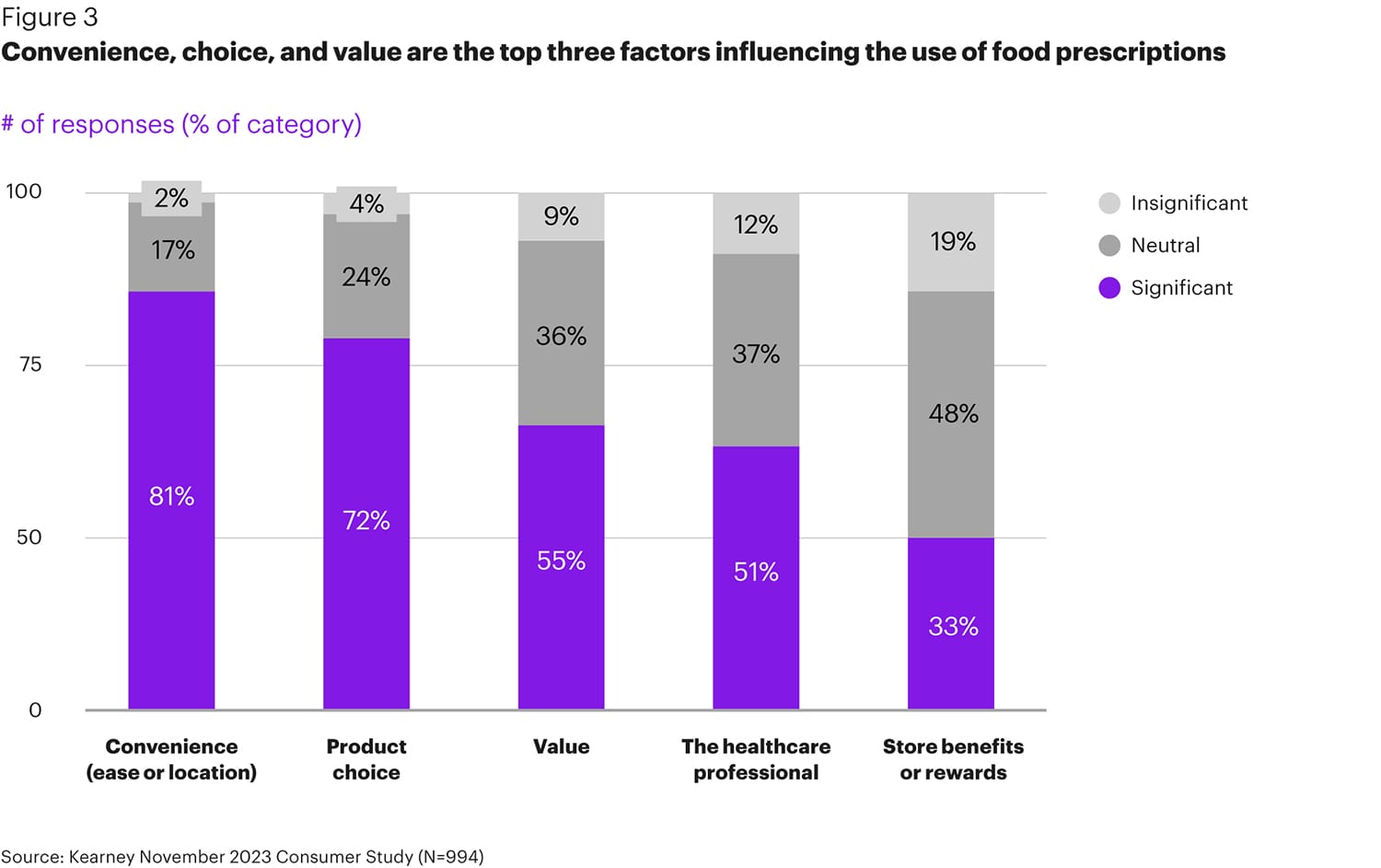
Of course, naming the program is only the first step. Our research also explored how to ensure patients take full advantage of the benefits of food-fueled health programs. When we asked consumers what they’d look for in a food prescription program, their top responses were convenience (diverse fulfillment locations), product choice and value (see Figure 3).
• Convenience — Consumers prefer to fill food prescriptions at grocery stores, but having a variety of fulfillment options will increase participation, especially among younger populations. Beyond grocery stores, consumers are open to filling food prescriptions at their pharmacies, specialty stores, or farmers’ markets or through delivery options.
• Product choice — Consumers are looking for a rich variety of fresh produce with diverse options that appeal to different tastes and dietary preferences. 72% of those we surveyed said variety was a “significant” factor in making a food prescription program appealing.
• Value — Finally, the program needs to deliver a high perceived value. The desired minimum voucher value varies by income, but a minimum voucher of $25 would satisfy 90% of consumers.
What is the pharmacy’s role in food prescriptions?
Pharmacies are uniquely positioned to support food prescription programs. Pharmacies are prevalent and embedded in communities, pharmacists strengthened their role as care providers during the pandemic, and many patients see a pharmacist more often than they see a doctor.
Food prescription awareness is highest among consumers who visit the pharmacy regularly, and this kind of program is most appealing to these pharmacy power users, too — signaling the key role that pharmacies can play in reaching these populations.
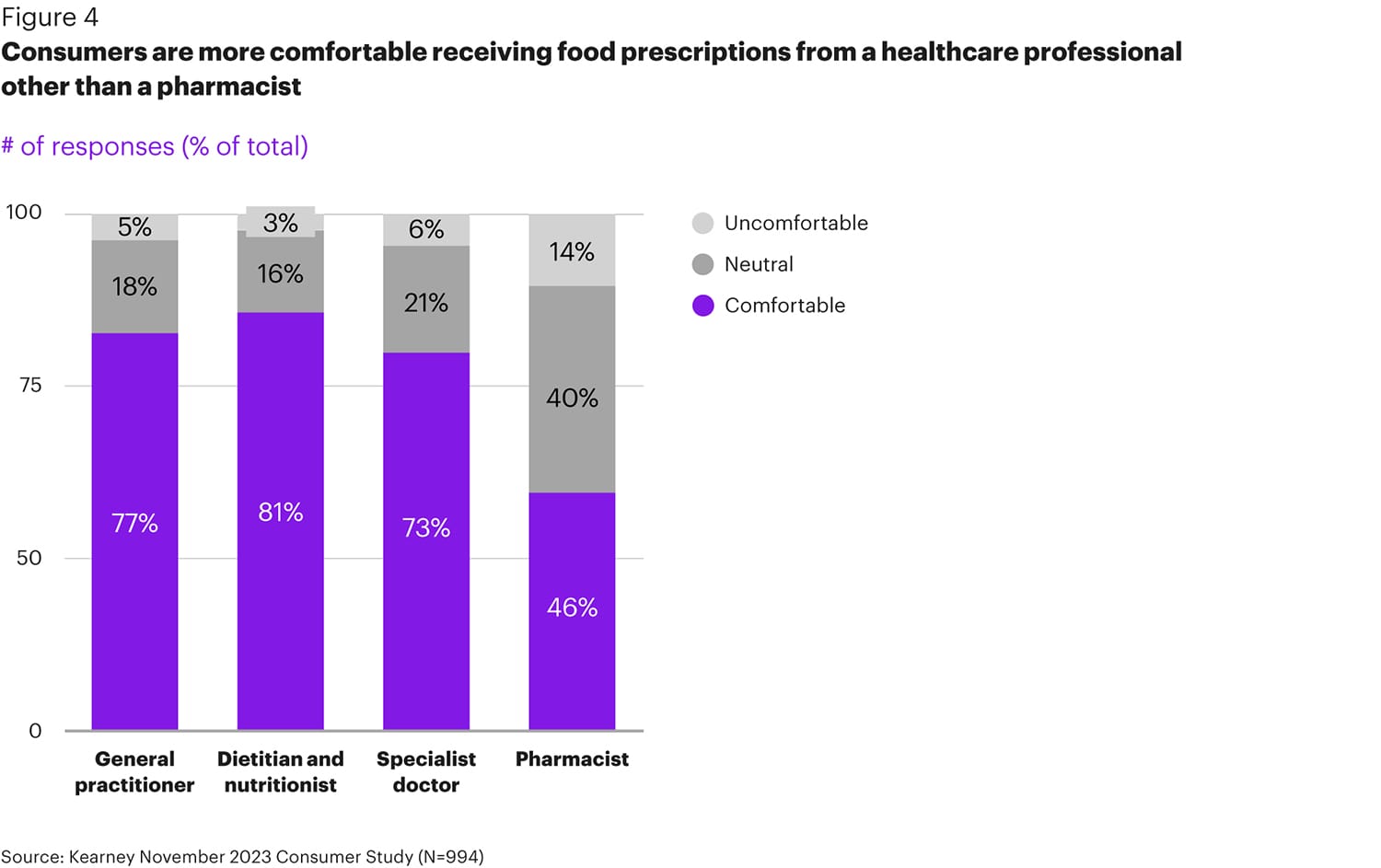
But will consumers look to pharmacists for diet advice? Our research shows that to be effective pharmacists will need to expand their role as part of the patient’s broader care team. In general, consumers said they’d prefer to receive food prescriptions from their general practitioner, dietitian, or specialist doctor (see Figure 4). But people who visit the pharmacy regularly, are lower income and are facing chronic illness are more comfortable with the idea of getting a food prescription from a pharmacist. As pharmacies evolve to be more future forward with an emphasis on primary care, there’s an opportunity to grow the role that pharmacies play in bringing food-fueled health to a broad population.
This data creates a call to action for pharmacies to develop a more consultative relationship with their customers. Pharmacists are well suited to play a role in patients’ health management since they understand the conditions and the nutrition that could improve patient outcomes. Educating consumers about nutrition, crafting careful messaging about pharmacies’ diet and nutrition management services, and building partnerships with other trusted health care professionals can help expand the role pharmacies play in this movement.
“There has been progress in the payment pathways and policy shifts to cover the cost of food for Food is Medicine interventions, and now we need to think more about covering the cost of Food is Medicine care,” says Holly Freishtat, senior director of Feeding Change at the Milken Institute. “This June, the Milken Institute will be publishing an action plan that highlights the importance of providing Food is Medicine care. It will identify key funding pathways, workflow operations, technology infrastructure and policies needed to successfully integrate Food is Medicine care in pharmacies.”
As food prescription programs gain traction and move toward scale, pharmacies should start thinking now about the role they can play in this growing movement and how they can start to engage their customers today.
Rodey Wing is a partner in the health practice at Kearney, a global strategy and management consulting firm. He can be reached at rodey.wing@kearney.com. Karen Yocky is a manager in the health practice at Kearney. She can be reached at karen.yocky@kearney.com.








