NEW YORK — Health care economists, health system leaders and policy makers have been talking seriously about measuring and paying for value in health care for more than a decade. Hospitals, clinics, pharmacies and practitioners across the country now are starting to move in that direction, incentivized since 2015 by Medicare’s adoption of alternative care models. However, the complete transformation from a system that prizes volume to a system that recognizes and pays for value will take decades. While paying for value is a relatively easy concept to understand, it is infinitely more difficult to execute.

Dan Leonard
Consider determining the value of biopharmaceuticals: There are organizations attempting to evaluate and measure the value of new drugs coming to the market. Those assessments often neglect or fail to capture the value of a medication over the full course of treatment. Value is even harder to capture when a single treatment can lead to a cure or a significant health improvement over a patient’s lifetime. Sometimes, we must look back at the historical arc of a disease or condition and the improvements that have been made over the years to get a comprehensive view of what brings value to patients.
Tracing health improvement and identifying the interventions that contribute to that improvement is exactly what the National Pharmaceutical Council (NPC), along with our research partners at RTI Health Solutions, sought recently to do. By looking retrospectively at the eight most serious diseases and conditions affecting Americans since 1990, and the interventions responsible for associated health benefits and improved outcomes, we have found another way to look at value — a construct that is defined by physicians. The research was recently published in the Journal of Managed Care and Specialty Pharmacy.
More than 130 experienced physicians were asked about which post-diagnosis innovations contributed to improved patient outcomes in treatment for such diseases as HIV, chronic obstructive pulmonary disease, lung cancer and depression. They responded by indicating the relative value of innovations in several areas:
• Pharmaceutical and biopharmaceutical: 56%.
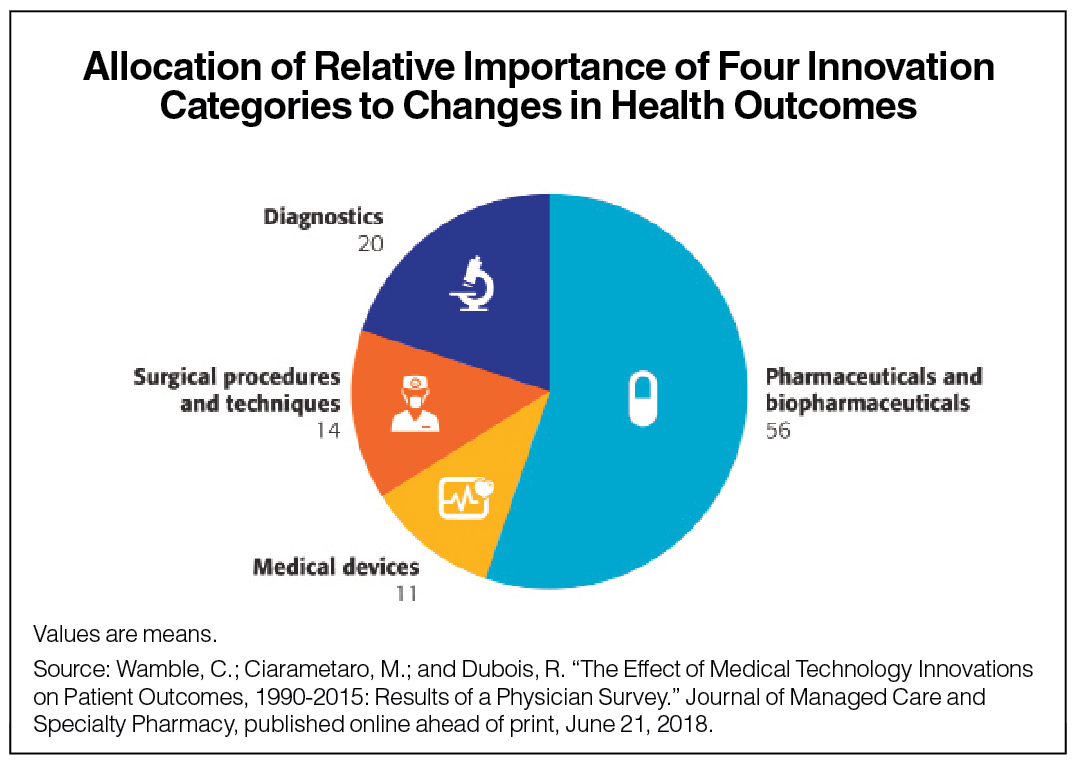
• Diagnostics: 20%.
• Surgical procedures and techniques: 14%.
• Medical devices: 11%.
Their responses favored biopharmaceutical innovation over other types by a factor of three in contributing to improvements in post-diagnosis mortality and morbidity outcomes over the evaluated period.
These findings provide an important perspective in the ongoing debate over the value of medical technology innovation. This is not surprising to us at NPC, where our members have been on the front lines of generating these innovations. Whereas an HIV diagnosis may once have equaled a death sentence, the disease is now manageable through medication. Similarly, many other serious conditions also are now being managed better through medications.
While the value of public health campaigns cannot be overestimated in reducing the incidence of such diseases as lung cancer by exposing the detrimental health effects of smoking, pharmaceutical and biopharmaceutical innovations are essential to the treatment of lung cancer patients, in many cases doubling their life expectancy.
All health care stakeholders must work together to move to a value-based system. While value-based principles might suggest that we should allocate scarce health care resources based on the benefit to the patient, as well as on the physician’s feedback, that is not what I am proposing. It is important to consider and capture the full value of interventions over time. The potential pitfall of attempts at assigning value to drugs or any individual component of the health care system is that they don’t capture the full value of what those interventions bring to the patient.
These are challenging, complex issues; truly understanding and leveraging a value-based system requires more nuance, not a single leap. Nevertheless, these findings illustrate that physician-perceived benefits provided by pharmaceutical and biopharmaceutical innovations are substantial when compared to other post-diagnosis innovations.
Dan Leonard is president of the National Pharmaceutical Council. He can be reached at dleonard@npcnow.org









