LITTLE ROCK, Ark. — Walgreens joined independent pharmacies at Monday’s Insurance & Commerce Senate hearing in Arkansas to address the critical issue of pharmacy benefit manager (PBM) practices and their impact on the viability of pharmacies across the country.
As an independent pharmacy, Walgreens faces many of the same reimbursement challenges as small, local pharmacies – often operating at a loss due to reimbursements that don't cover the actual costs of purchasing and dispensing medications. PBM consolidation has created an uneven playing field, jeopardizing access to pharmacy care for millions of patients. Walgreens is supporting Arkansas’ proposed regulation (rule 128), which would require reimbursement that is no less than the true cost to purchase and dispense drugs.
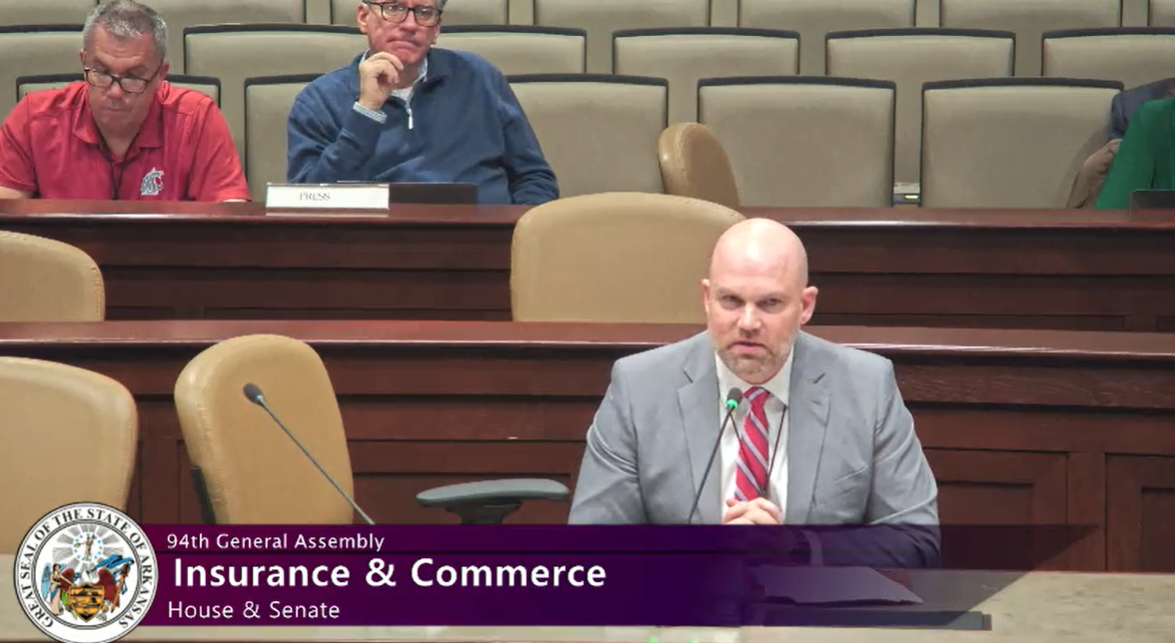
“Pharmacies like Walgreens play a critical role in ensuring patients receive the medications and care they need, particularly in underserved and rural areas where options are already limited. However, PBM practices, such as unfair reimbursement rates and steering, are jeopardizing pharmacy access, making it harder for pharmacies to keep their doors open," said Brad Lawson, healthcare supervisor, Western Operations, for Walgreens during the hearing. "Rule 128 is an essential step toward leveling the playing field and protecting the trusted healthcare services pharmacies provide to communities across Arkansas and beyond," he added.
Key points that Lawson from Walgreens addressed included:
- The financial pressures and impact from PBM reimbursement practices on the viability of community pharmacy.
- How current practices, including "spread pricing" and patient steering, threaten pharmacy access in underserved communities.
- The urgent need for Rule 128 in Arkansas to ensure fair reimbursement and patient choice.








